In 2026, the radiology AI conversation is shifting from “Which algorithm is best?” to “How do we run AI in production without creating new risks or new bottlenecks?” Hospitals and imaging leaders are under pressure to improve turnaround times, reduce backlogs, and keep quality consistent—yet everyone knows that technology layered onto an already complex workflow can backfire if it isn’t governed properly.
The most successful AI programs aren’t defined by a single tool. They’re defined by governance, interoperability, and measurable performance—and by a workflow design that supports radiologists rather than fragmenting their attention.
Why AI success looks different in 2026
Early AI adoption often focused on point solutions: a triage tool here, a detection aid there. Today, organizations want outcomes: faster reads, fewer misses, more consistent reporting, and fewer operational disruptions. That’s why governance is taking center stage. The American College of Radiology (ACR) has emphasized the need for formal AI governance and oversight structures to keep patient safety and reliability at the forefront.
At the same time, the industry is pushing hard on interoperability—making sure AI tools integrate into PACS/RIS and clinical communication rather than living in “yet another dashboard.” RSNA has showcased how workflow integration and standards can reduce friction points and help AI support real clinical scenarios.
The 2026 AI governance checklist (simple, practical, usable)
Whether you’re adopting your first tool or scaling across modalities, governance doesn’t need to be complicated—but it does need to be real. A strong governance model typically includes:
1) Clear clinical ownership
AI cannot be “owned by IT.” Radiology leaders should define:
-
Where AI is allowed to influence priority or interpretation
-
When radiologists can override AI outputs (and how overrides are documented)
-
What happens when AI and clinical suspicion conflict
2) Validation before scale
Before broad rollout, validate performance in your setting:
-
Scanner/protocol differences
-
Patient population differences
-
Volume and study mix differences
Even a great algorithm can underperform when protocols change or volumes surge.
3) Ongoing monitoring for drift
AI isn’t “install and forget.” Real-world performance changes over time—new scanners, new protocols, and shifting patient demographics can all cause drift. That’s why long-term monitoring is a growing focus in radiology AI standards efforts. For example, ACR has discussed practice parameters and programs aimed at integrating AI safely into clinical practice.
4) Operational metrics that matter
Track the metrics your hospital actually feels:
-
ED and inpatient turnaround time (TAT)
-
Backlog hours by modality
-
Discrepancy rates and peer-review signals
-
Percentage of cases escalated via triage
-
Radiologist interruption load (alerts, worklist reshuffles)
If AI improves one metric by harming another, it’s not a net win.
Where Vesta fits: AI + subspecialty reads + QA
For many hospitals, the most practical 2026 strategy isn’t “AI replaces humans.” It’s AI improves routing and prioritization, while subspecialty radiologists deliver the interpretation quality that clinical teams depend on.
A common best-practice workflow looks like this:
-
AI supports triage and worklist prioritization (especially for time-sensitive pathways)
-
Subspecialty radiologists provide consistent, high-confidence reads
-
QA processes (peer review, discrepancy tracking, feedback loops) ensure reliability over time
That combination is how you get the real goal: speed and confidence together—not speed at the expense of quality.
What to do next
If you’re building or refining an AI program in 2026, start with your workflow map—then add tools where they reduce friction. And make sure governance is designed before adoption accelerates.
If your team needs scalable subspecialty coverage to support operational goals (nights/weekends, overflow, or targeted service lines), Vesta Teleradiology can help you build a coverage model that keeps reads moving without sacrificing consistency. Learn more at https://vestarad.com.


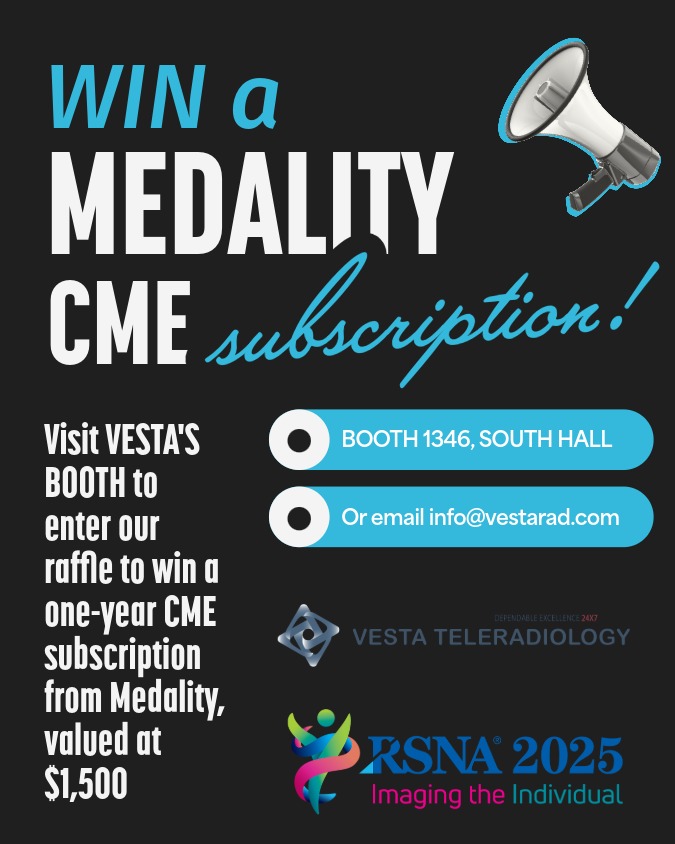 Why this RSNA prize matters for teams—not just individuals
Why this RSNA prize matters for teams—not just individuals