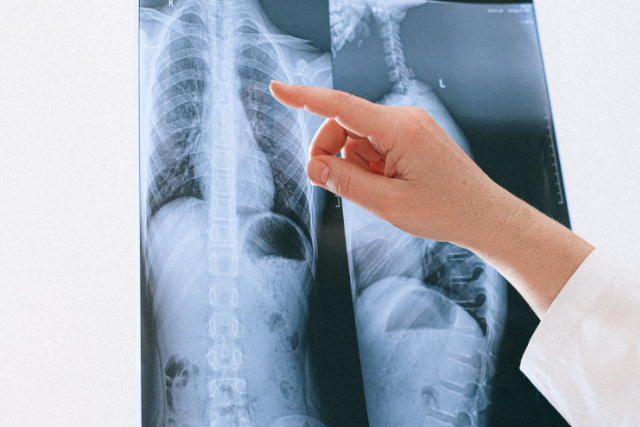
Access to quality healthcare in rural areas can be a significant challenge. For communities in Illinois and Ohio, where many rural hospitals and outpatient centers serve as lifelines, ensuring timely and accurate radiological services is crucial. As a teleradiology company, we specialize in bridging this gap by offering high-quality diagnostic imaging interpretation, ensuring rural healthcare providers can deliver top-tier care to their patients.
Recent Developments in Healthcare Laws Impacting Illinois and Ohio
- Medicare Reimbursement Changes (2025)
Rural hospitals in Illinois and Ohio, many of which rely heavily on Medicare funding, continue to face challenges with reimbursement rates. Adjustments to the Medicare Physician Fee Schedule have historically impacted imaging services, including reductions in the professional component payments for certain procedures like X-rays and MRIs. These changes highlight the importance of cost-effective solutions for maintaining high-quality care.
To mitigate these challenges, teleradiology services like ours play a vital role. By reducing overhead costs associated with maintaining in-house radiologists, rural hospitals can ensure uninterrupted imaging services without compromising care quality.
2. Breast Density Notification Laws
Starting in September 2024, new breast density notification requirements took effect nationwide, including Illinois and Ohio. Radiologists must inform patients if they have dense breast tissue, a factor that can obscure mammogram results and increase cancer risks. Rural facilities are updating workflows to comply with these laws. Our teleradiology service assists hospitals by streamlining compliance and ensuring accurate reporting.
Source: FDA
- Federal Funding for Rural Healthcare
Both Illinois and Ohio benefit from federal programs like the Rural Health Care Program, which provides funding to improve telehealth infrastructure. These grants enable rural hospitals to adopt advanced diagnostic imaging solutions, making it easier to integrate teleradiology into their systems.
Source: FCC Healthcare Connect Fund
The Role of Teleradiology in Rural Cities
Illinois: Supporting Rural Communities
Illinois is home to numerous rural towns such as Monmouth, Galena, and Princeton. These communities rely on critical access hospitals (CAHs) to serve their populations, which often face higher rates of chronic illnesses and limited access to specialists. Teleradiology addresses these challenges by providing:
- 24/7 Imaging Support: Our services ensure that even small hospitals can deliver around-the-clock diagnostic imaging interpretations.
- Subspecialty Expertise: From musculoskeletal imaging to neuroimaging, we offer specialized radiology services that are typically unavailable in rural areas.
 Ohio: Enhancing Care in Rural Towns
Ohio: Enhancing Care in Rural Towns
Ohio’s rural landscape includes cities like Portsmouth, Gallipolis, and Defiance. Many of these areas face shortages of medical professionals, particularly radiologists. Our teleradiology services support these communities by:
- Faster Turnaround Times: Critical imaging results are delivered quickly, helping providers make timely treatment decisions.
- Cost Savings: Rural hospitals save significantly by outsourcing radiology needs rather than maintaining full-time staff.
Challenges Facing Rural Healthcare
Rural hospitals in Illinois and Ohio grapple with workforce shortages, aging populations, and rising operational costs. However, partnerships with teleradiology companies can alleviate these burdens by:
- Expanding Diagnostic Capabilities: We enable even the smallest hospitals to offer advanced imaging interpretations.
- Improving Patient Outcomes: Accurate and timely diagnoses lead to better treatment plans and improved patient care.
- Reducing Physician Burnout: Remote radiology support alleviates the workload for overburdened rural providers.
Vesta Teleradiology 24/7 Support for Rural Hospitals and Outpatient Centers
Rural hospitals and outpatient centers in Illinois and Ohio are vital to the health of their communities. By leveraging teleradiology services, these facilities can overcome the unique challenges of providing quality care in underserved areas. Our company is proud to partner with these hospitals, offering expert radiology interpretations and helping ensure patients in rural cities receive the care they deserve.
For more information about how we can support your healthcare facility, reach out to us today.


 Implications for Healthcare Providers
Implications for Healthcare Providers
 What types of work environments are available for radiologists?
What types of work environments are available for radiologists? What should I consider when evaluating a job offer?
What should I consider when evaluating a job offer?

 However, challenges remain, including concerns about transparency in AI decision-making and biases in data sets. These hurdles are gradually being addressed with stricter regulations and improved algorithm training. AI isn’t just a tool; it’s becoming a trusted collaborator in radiology practices worldwide.
However, challenges remain, including concerns about transparency in AI decision-making and biases in data sets. These hurdles are gradually being addressed with stricter regulations and improved algorithm training. AI isn’t just a tool; it’s becoming a trusted collaborator in radiology practices worldwide. Radiology practices are adapting to these regulations by enhancing their reporting systems and educating patients about the implications of breast density. This legislation empowers patients to make informed decisions about supplemental screening options, improving early detection and outcomes.
Radiology practices are adapting to these regulations by enhancing their reporting systems and educating patients about the implications of breast density. This legislation empowers patients to make informed decisions about supplemental screening options, improving early detection and outcomes.




