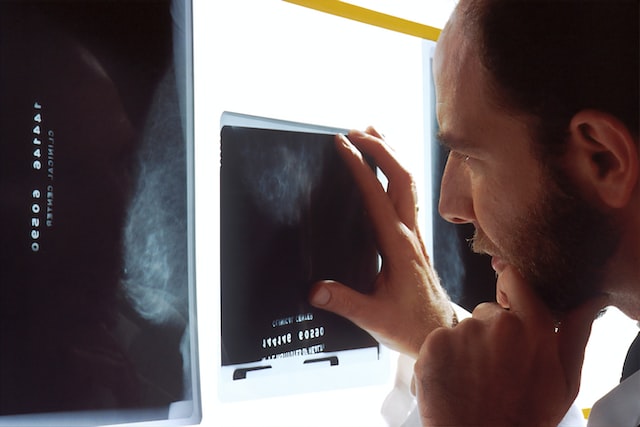
The healthcare market is experiencing a shift towards outpatient care, driven by reimbursement changes, pandemic effects, and patient preferences, particularly prominent in the U.S. Providers are diversifying into sub-specializations like neurology and oncology, raising the demand for advanced imaging like MRI and CT. This trend has led to increased utilization of outpatient imaging and teleradiology services.
By the NuMbers
Diagnostic imaging is becoming increasingly crucial in healthcare, with the market projected to reach $31.9bn in 2023 and grow at a 4.8% CAGR to $45.8bn in 2030. The rise is driven by chronic diseases, an aging population, and post-Covid-19 demand recovery. To meet this demand, companies are focusing on advanced and accessible technologies, such as handheld ultrasounds. About 1,949 imaging devices are in development, with 112 expected to gain approval in 2023.
According to Fortune Business Insights, in 2022, the computed tomography (CT) segment held the largest market share due to a rise in CT scan procedures and higher average pricing. For instance, OECD data for 2021 showed 84.5 million CT scan procedures in the U.S., up by 15.8% from the previous year. The growing geriatric population has also contributed to increased demand for CT scans.
Key Players
Key players include GE Healthcare, Philips, Siemens Healthineers, and more. Challenges include high equipment costs and a shortage of skilled personnel, impacting accessibility and patient care quality. Opportunities arise from the growing demand for imaging services, especially for chronic diseases, and the development of new modalities like 3D mammography and MRI-guided focused ultrasound. Emerging economies like India, China, and Brazil are pivotal, driven by rising chronic diseases. Major players like Siemens Healthineers are expanding in these markets. Additionally, teaching hospitals are increasing demand for advanced imaging methods to enhance patient care.
Your Dedicated Radiology Partner: Vesta
Partnering with Vesta as your radiology partner ensures access to accurate and timely imaging interpretations and readings for subspecialties. Whether you are an outpatient imaging center or traditional hospital, our collaboration offers a seamless and efficient experience. Trust us to be your reliable radiology partner, empowering you with the insights and tools needed for improved healthcare outcomes.
 Sources:
Sources:
Itnonline.com
Medicaldevices-network.com
fortunebusinessinsights.com
openai.com