The U.S. Food and Drug Administration issued a warning to consumers on July 17 about avoiding the use of ultrasound devices from a Texas-based manufacturer and distributor called RoyalVibe Health.
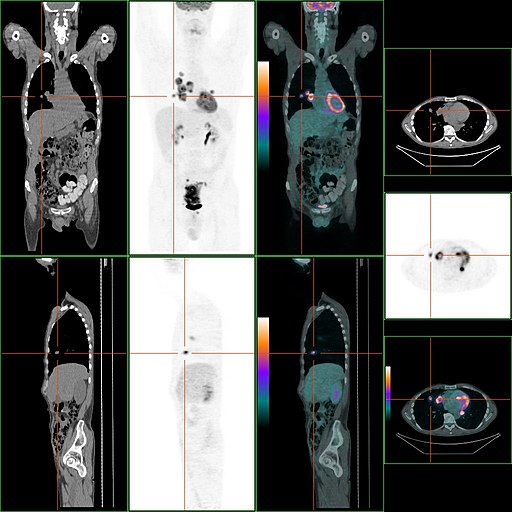
The company sells direct-to-consumer ultrasound scanners, marketing them to be used for various medical purposes, including diagnosing and treating serious conditions like cancer, diabetes, heart disease, Parkinson’s, and depression. However, the FDA has not reviewed these devices, and they lack the necessary 510(k) clearance or premarket approval.
What is 510(k) Clearance?
The 510(k) clearance is a regulatory pathway used by the U.S. FDA to evaluate and approve medical devices. If a new medical device is deemed substantially equivalent to a legally marketed device (known as a “predicate device”), the manufacturer can submit a 510(k) premarket notification to the FDA. The FDA reviews the submission to ensure the new device shares the same intended use and technology as the predicate device. If approved, the new device receives 510(k) clearance, allowing it to be marketed in the U.S. The 510(k) process is commonly used for moderate-risk medical devices and relies on the safety record of similar, already-approved devices to expedite approvals while ensuring safety and effectiveness.
Ultrasound Therapy
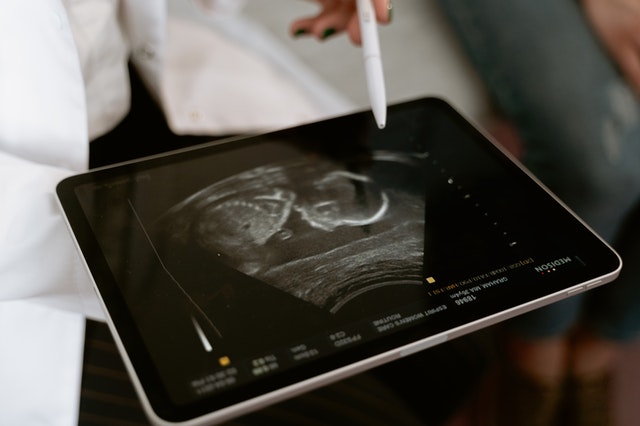
Ultrasound therapy is a non-invasive medical treatment that utilizes high-frequency sound waves to target specific tissues in the body. During the procedure, a handheld device emits these sound waves, which penetrate the skin and cause vibrations at a cellular level. This treatment process is believed to increase blood flow, relax muscles, and promote tissue healing. Ultrasound therapy is commonly used by physical therapists to alleviate pain, reduce inflammation, and improve tissue mobility in conditions like muscle strains, joint injuries, and certain musculoskeletal disorders. It is a safe and effective treatment that can provide relief and aid in the recovery process for various injuries and conditions.
Open Communication with Patients
Unfortunately, some consumers find products on the market that they can purchase directly in hopes to use for at-home self-care. Please advise your patients to be wary of these types of devices, including the products the FDA has not approved such as RoyalVibe Health. Patient education can go a very long way, so it is important to address their questions about their health, pain and concerns and emphasize that treatment should be administered by their healthcare provider.
Sources:
Fda.gov
verywellhealth.com
radiologybusiness.com
openai.com







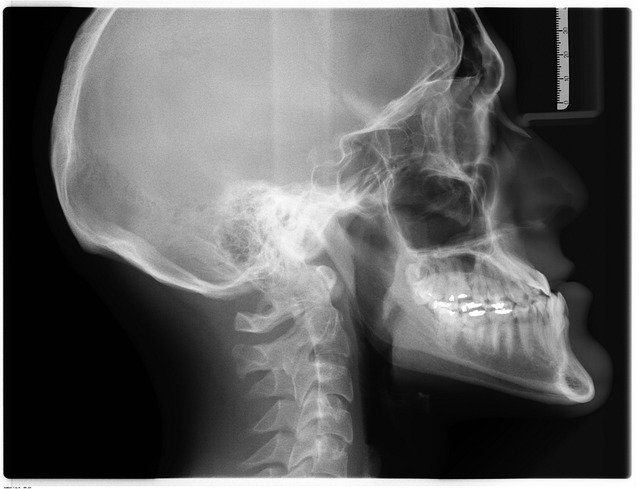 Going back to the beginning, the first X-ray picture in 1895 by
Going back to the beginning, the first X-ray picture in 1895 by
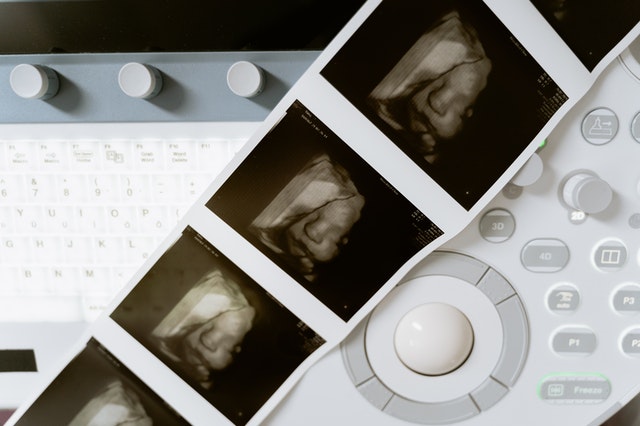 Fun Fact: the 3-D ultrasound actually takes thousands of photos at once to create a 3d image that is extremely clear.
Fun Fact: the 3-D ultrasound actually takes thousands of photos at once to create a 3d image that is extremely clear.
 Studies suggest
Studies suggest
