When experts study health across various U.S. demographics, one particular metric often falls into sharp relief: there is a significant health burden weighing on American Indians and Alaska Natives. The AI/AN population accounts for about 9.7 million people in the United States (about 2.9% of the population), and this group routinely ranks near the bottom for life expectancy, insurance coverage, and overall health (both mental and physical).
About 2.6 million of AI/AN people receive healthcare services from the IHS, or Indian Health Services. This program aims (to use their own words), “to raise the physical, mental, social, and spiritual health of American Indians and Alaska Natives to the highest level,” but is the program succeeding? Let’s examine the IHS and its mission, challenges, and efficacy.
The IHS Story
While the U.S. government and federally recognized tribes have worked in partnership to provide AI/AN people with healthcare since the 1700s, the IHS officially began its work in July of 1955. The organization first worked to build hospitals in remote parts of the country that served Native individuals in the area; over the years, the IHS has expanded its efforts to include both health services and public health education.
Today, the IHS is a part of the U.S. Department of Health and Human Services. They operate more than 600 medical facilities on or near Indian reservations across 37 states, and they also work to tackle challenges impacting AI/AN public health.
Challenges Facing the IHS
There’s no arguing that the IHS has laudable goals and that its team of 15,000 employees works hard to improve AI/AN lives. But IHS still faces significant challenges in its efforts. Research shows that about 61% of IHS medical buildings are in “fair” or “poor” conditions, which severely limits medical professionals’ ability to treat their patients. Similarly, many IHS facilities report working with broken or unreliable equipment, which affects the standard of care they can provide.
Furthermore, many IHS buildings are located in remote, rural locations with few amenities like grocery stores, schools, or even adequate housing. This makes recruiting and retaining medical staff especially difficult and limits the pool of quality professionals willing to practice in their network (notably, 50-75% of physicians who contact IHS recruiters have conduct or licensure issues on their record).

Despite these challenges, the IHS continues to make changes that benefit AI/AN peoples across the country. For example, in 2022 the IHS fought to secure $3.5 billion in funding from the government that allowed them to improve water supplies and wastewater disposal systems on tribal lands. Efforts like these help American Indians and Alaskan Natives improve their health and enjoy a better quality of life, and they prove that organizations like the IHS offer a tremendous benefit to the people they serve.
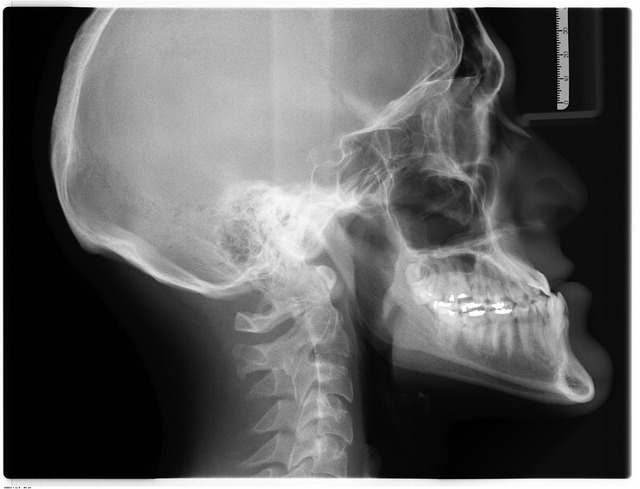
Teleradiology Support for IHS
Ensuring all populations in the US receive adequate care is the goal of your healthcare facility. Vesta is here should you find yourself short staffed for radiologists—we have U.S. Board certified radiologists available for preliminary and final interpretations whenever you need it. In fact, Vesta is already proving teleradiology services to several IHS sites. Please reach out to us to learn more:
Vesta Teleradiology 1071 S. Sun Dr. Suite 2001 Lake Mary, FL, 32746
Phone: 877-55-VESTA









 Sources:
Sources: