New Research by Harvard Medical School, MIT and Stanford on AI and Clinician Performance
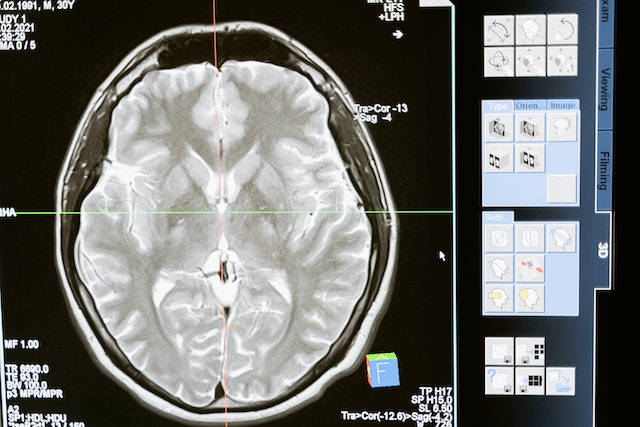
The potential of medical artificial intelligence (AI) tools to enhance clinicians’ performance in interpreting medical images varies among individual clinicians, as highlighted by recent research led by Harvard Medical School, MIT, and Stanford. Published in Nature Medicine, the study underscores the intricate nature of human-AI interaction, which remains incompletely understood. While some radiologists benefit from AI assistance, others experience interference, affecting diagnostic accuracy.
The findings stress the necessity for personalized AI systems tailored to individual clinicians, emphasizing careful implementation to maximize benefits and minimize harm. Despite variations in AI’s impact, the results shouldn’t deter AI adoption but rather prompt a deeper understanding of human-AI dynamics to design approaches that enhance human performance.
To ensure effective integration of AI in clinical practice, collaboration between AI developers and clinicians is essential, alongside rigorous testing in real-world scenarios. Furthermore, efforts should focus on improving AI accuracy and training radiologists to discern AI inaccuracies, facilitating informed decision-making. Ultimately, understanding the complexities of machine-human interaction is pivotal for optimizing patient care through AI integration in radiology.
AI and Workflows
New research highlights a novel reporting workflow that automatically incorporates artificial intelligence (AI) findings into structured radiology reports, streamlining physicians’ tasks and saving valuable time. German experts shared their experience with the “AI to SR pipeline,” which integrates a commercially available AI tool for chest X-ray pathology detection and localization into structured report templates.
In evaluations conducted at University Medical Center Mainz, expert radiologists found that reports generated using the AI to SR pipeline were faster compared to free-text reporting and conventional structured reporting. Additionally, subjective quality assessments indicated higher ratings for reports created with the pipeline.
In the hospital’s clinical routine, chest X-ray images are sent to the picture archiving and communication system, then automatically forwarded to the AI tool for analysis. The results are output in a DICOM structured reporting format, taking approximately five minutes from image acquisition to final reporting. Radiologists were able to create chest X-ray reports significantly faster with the pipeline compared to free-text and conventional structured reporting, while also rating the AI-generated reports more favorably.
The authors suggest that this AI-driven reporting pipeline offers standardized, time-efficient, and high-quality reporting for chest X-rays, potentially enhancing AI integration into daily clinical practice and maximizing its benefits.
Sources:
Medicalxpress.com
Radiologybusiness.com
Openai.com