The AAMC (Association of American Medical Colleges) has released new projections indicating a physician shortage of up to 86,000 physicians in the United States by 2036. This underscores the critical need for sustained and increased investments in training new physicians to address the country’s healthcare needs. The report, conducted by GlobalData Plc, includes various scenarios based on trends in healthcare delivery and the workforce. While the projected shortfall is smaller than previous estimates, it still highlights the necessity for additional investments in graduate medical education (GME). Demographics, particularly population growth and aging, are driving the increasing demand for physicians. The report also notes a significant portion of the physician workforce nearing retirement age, which will further decrease the physician supply. Addressing underserved communities could require approximately 202,800 more physicians than current estimates. Lifting the federal cap on Medicare support for GME and bipartisan legislation like the Resident Physician Shortage Reduction Act aim to alleviate the shortage, but further efforts are needed to meet future healthcare demands.
Rural Americans’ Healthcare Challenges
Rural Americans face significant healthcare challenges, with fewer available doctors compared to urban areas, exacerbating existing health issues. Dr. Bruce A. Scott, President of the American Medical Association, emphasizes the urgent need for policymakers to address these disparities. Rural communities experience higher rates of various illnesses, exacerbated by economic pressures and limited access to healthy living conditions. The shortage of specialists and the closure of rural hospitals further compound the problem. Insufficient access to primary care physicians is a pressing issue, with inadequate residency spots and decreasing applications from rural areas. The AMA advocates for changes to the Medicare physician payment system, which has seen a decline in rates over the years. Administrative burdens, such as prior authorizations, are also contributing to physician burnout and compromising patient care. To combat the doctor shortage and rural health challenges, the AMA advocates for healthcare reforms, including overhauling the Medicare payment system, expanding telehealth, increasing residency positions, incentivizing rural practice, and addressing workforce stresses.
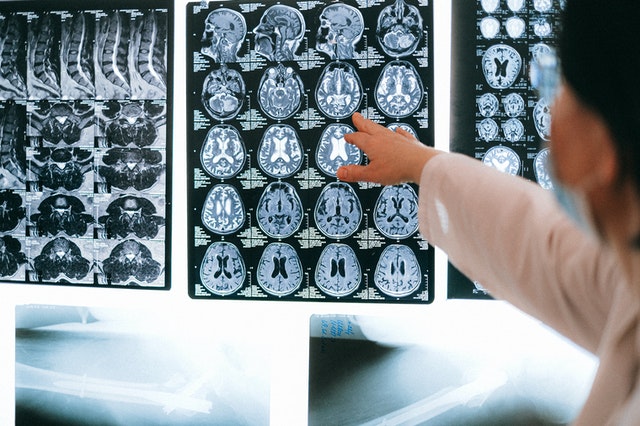
Radiology Is Being Hit, Too
Radiology departments are grappling with worsening staffing shortages alongside declining reimbursements. During the RSNA 2023 meeting, Ashish Sant from Merge by Merative discussed key trends and challenges. Staffing and cost management remain top concerns due to burnout and insufficient replacements for retiring radiologists. To address these issues, there’s a push towards cloud-based solutions, with a modular approach easing concerns about data security and patient information management. The pandemic has accelerated the shift towards cloud adoption, highlighting benefits such as accessibility and cost reduction. Integrating AI into radiology workflows is another focus, though challenges persist in seamlessly embedding AI solutions. Merge’s partnership with Microsoft Azure aims to provide customers with cloud solutions tailored to their needs.
Radiology Support for the US
Addressing radiology staffing shortages is crucial for ensuring efficient and effective healthcare delivery. Whether you’re a hospital, outpatient center, or part of the Indian Health Service (IHS), Vesta is here to help. Our team can provide on-site radiologists or teleradiologists to meet the specific needs of your facility. By partnering with us, you can ensure timely and accurate radiology services, ultimately improving patient care and outcomes. Don’t let staffing shortages hinder your operations – reach out today to learn how we can support your radiology department.
Sources:
Aamc.org
dtnpf.com
Healthimaging.com
openai.com















 Sources:
Sources: