The fields of science and medicine are always progressing. This progression intends to help both patients and providers.
Today, artificial intelligence (AI) is becoming common as a way to diagnose patients. It provides a more efficient way to collect and store information. The software can even analyze imaging to a high level of accuracy. This helps providers catch a problem that they may have missed before.
AI is a field that is advancing quickly. What progress have we seen in the past couple of years? What programs have we begun to put in place?
What Is Artificial Intelligence?
Artificial intelligence refers to highly advanced computers or computer-controlled robots. These computers are capable of performing incredibly complex tasks. Before, we thought these tasks could only be done by intelligent beings.

These computers are often associated with human characteristics. They seem to be able to reason and learn from past experiences.
How Is Artificial Intelligence Used For Diagnostic Imaging & Radiation?
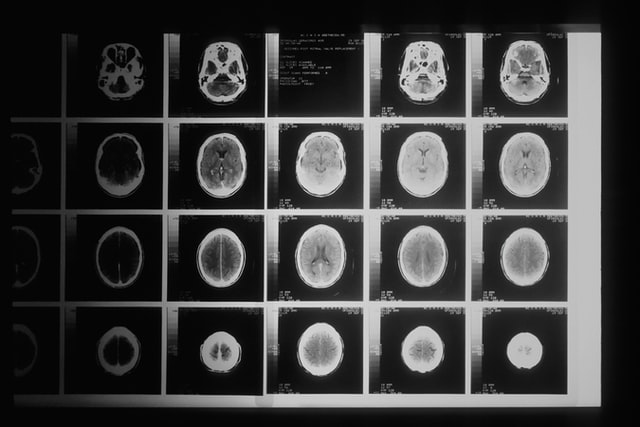
Using AI in radiology and imaging has been gaining traction in the medical world. We use it largely to store and analyze data, helping physicians to make a prognosis. AI can store and analyze all a patient’s records. It can then make a diagnosis based on those records. The analysis is often far more accurate than what a human counterpart can do.
The use of AI is also helpful because of its storage capability. AI can have large imaging biobanks to hold more images than standard computers.
It also makes the lives of physicians easier by filtering patients by need. It can recommend appropriate diagnostic imaging based on the patient’s current records. It can also sort patients by priority in the case of an emergency.
What Advancements Have Been Made?
AI means to eliminate problems associated with human limitations. Traditional imaging takes a team of technicians. They must take the imaging as well as interpret it. This can be time-consuming. Plus, AI is able to analyze images with far greater accuracy than the human eye.
Radiomics
Radiomics is a tool that performs a deep analysis of tumors down to the molecular level. AI can perform radiomics with far better accuracy than the human eye or brain.
AI can analyze a specific region and extract over 400 elements. It then takes these features and correlates them with other data to form a diagnosis. The AI can analyze features from radiographs, CT, MRI, or PET studies.
Rapid Brain-Imaging AI Software
Hyperfine is the manufacturer of portable MRI machines. They are now creating these machines with new AI intelligence software. They believe that this new software will be able to perform brain scans in under 3 minutes.
AI-Generated Drugs
In 2020, an AI-created drug went to human clinical trials. The drug intends to treat OCD, and was designed entirely by AI. Exscientia is the manufacturer of the drug. They say that it normally takes about 4.5 years to get a new drug to this stage of testing. With AI generation, the drug got to the human clinical trial stage in under 12 months.
Making A Diagnosis
We stated earlier that AI is being used as a way to more efficiently diagnose patients. Still, relying entirely on AI to do this can complicate things and may be unwise.
So, the researchers of MIT’s Computer Science and Artificial Intelligence Lab worked to combat this. They created a machine learning system that analyzes the data and decides whether to diagnose.
If it “feels” it’s unable to make an accurate prediction, it will defer to a medical professional. It even considers whether to defer to an expert based on who in the medical team is available. It will consider each team member’s availability, level of experience, and specialty.
Conclusion
AI in diagnostic imaging shows promise to truly advance quality of care for patients. We are excited to see more advancements in this arena. In the meantime, we don’t believe any machine can currently replace a trained human eye when it comes to interpretations. At Vesta, we provide US Board Certified radiologists who work to provide accurate preliminary and final interpretations. Learn how we can support your radiology department– contact us today.