The United States spends 2.7 trillion dollars annually on healthcare, more than any other country. The Affordable Care Act, (ACA) when it was signed into law in 2010, attempted to make that landmark first step, in providing universal healthcare available to all. Though the ACA was enacted in 2010, only certain provisions were in place at it’s inception. The full force of the multi-pronged strategic manifesto, that is the Affordable Care Act, were not truly a reality until 2013. Given the relatively short time frame in which to gather outcomes data, only very specific subsets of data are available upon which to draw conclusions. This is not unexpected however, and as more time passes under the ACA, information will continue to trickle in. In much the same way that the hallmark Medicare Act and implementation in 1965, when Medicare was enacted,one would expect that universal healthcare coverage of an older population, with more chronic illness, would give rise to a tsunami of health outcomes data. That was simply not the case, data trickled in, and now 50 years later, the Medicare Program is the yardstick by which all parameters within healthcare are measured. With the passage of time we will have a much larger pool of data to draw upon to measure the true successes or failures of the Affordable Care Act in achieving its goals.
Though the data is sparse, there have been several overarching achievements. Among them, an uninsured population is at the lowest level in years, there is improved access to care and utilization of services, as well a significant decrease in the financial burden faced by hospitals for uncompensated care. Two specific areas that have been studied in further depth involve two programs, for which we have specific data with defined health indices.
An area that has received quite a bit of attention, for several reasons and has the most actual disease specific statistical data, is a provision under the Affordable Care Act, known as Medicare’s Hospital Re-admissions Reduction Program ( HRRP). This was one of the promised Medicare reform measures, promised under the ACA. Within this program, Medicare provides financial incentives to hospitals who lower readmission rates for common illnesses seen in this population. Specifically,it measures readmission for Myocardial Infarction, Congestive Heart Failure, Pneumonia, Chronic Obstructive Pulmonary Disease, as well as post-surgical re-admissions for complications of elective Knee and Hip Arthroplasty or replacement. Data has gathered across the country at all hospitals and readmission rates were measured and data accumulated. Readmission was defined as readmission to a hospital within 30 days.
Historically, one in five Medicare patients are readmitted within 30 days of discharge. An estimated three-quarters of these re-admissions were considered preventable. Beginning fiscal year 2013, the hospitals in violation of the Hospital Re-admissions Reduction Program, who had a substantial number of “bounce-backs” or early re-admissions for conditions that fell within the measured indices ( MI, CHF,Pneumonia, COPD, and most recently, post op knee and hip replacements with complications) were levied heavy penalties. Since it’s 2013 inception, the HRRP has penalize some 2,200 hospitals. According to a report in Health Affairs, the sum aggregate of these penalties has resulted in 280 million dollars in Medicare payments, by the penalized hospitals.
There is reason to believe that the new HRRP provision has had a positive effect in lowering hospital readmission rates, and will continue to show improvement as hospitals institute protocols to meet these goals, and this is good the patients. The CMS, Center for Medicare and Medicaid Services, Medicare’s governing body, reported a 17.8% decrease in re-admissions, which translates to roughly 70,000 fewer patients readmitted within 30 days of discharge. Given that presumptively three-quarters of these admissions are preventable, further strategies are directed on ways for patients to receive improved aftercare, where early indicators of disease exacerbations, decompensation or wound infections, could be diagnosed and treated promptly, prior to requiring hospital readmission.
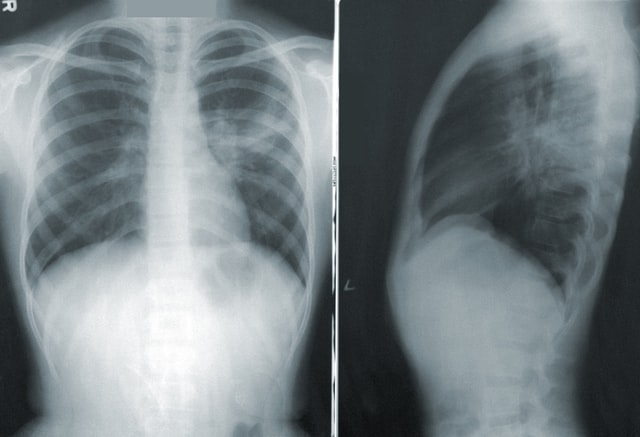
The ACA promises to utilize novel approaches and provide transparency in improving compliance HRRP initiatives. Recognition of early indicators of patient decompensation is not a novel concept. However, novel modalities can be utilized to meet this goal. Newer technologies such as teleradiology services and telemedicine may provide an avenue for early recognition of symptoms and prompt management, prior to incurring a HRRP penalty. In this population, many go to skilled nursing facilities upon discharge, where symptoms which can be accessed clinically and confirmed, with mobile radiology services, such as those provided by Vesta’s professional staff. Congestive Heart Failure, Pneumonia, and Chronic Obstructive Pulmonary Disease diagnoses can be readily achieved with a simple chest radiograph. Catching an early pneumonia before the patient has respiratory compromise or worse, sepsis, and requires readmission, could be so easily achieved with the convenience of mobile .teleradiology groups and an inexpensive chest x-ray.
Providers of teleradiology services, such as Vesta, provide professionally trained staff and seasoned radiologists who can provide prompt interpretation of films and mean the difference between missing a diagnosis, and risking failure on one of the HRRP monitored diseases. This seems an extremely reasonable, convenient and cost effective measure, that could be implemented to prevent hospital readmissions. Proving both beneficial in optimizing patient care as well as avoiding a HRRP penalty. Additionally, given the HRRP required transparency, the multiple levels of Quality Assurance measures, implemented by Vesta, would make compliance a simplified process.
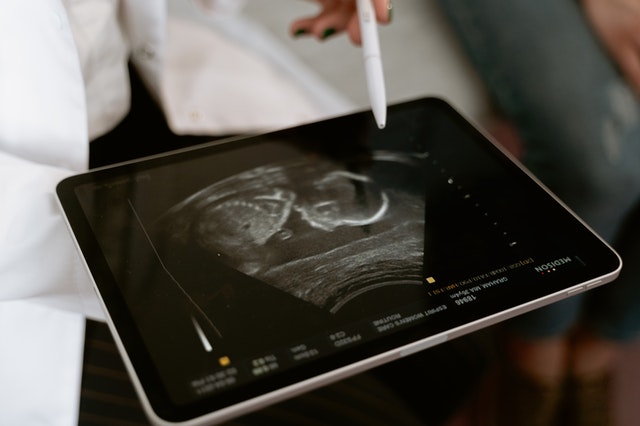
In late 2014, the HRRP was expanded to include re-admissions for complications of elective total knee and hip replacements. These complications again can be readily diagnosed with plain radiographs. Ultrasonography services, also offered by Vesta’s menu of mobile services ,can also be useful in determining the location of an infected hematoma or joint abscess, as well as ruling out deep vein thrombosis, a risk factor after all lower extremity orthopedic surgeries. If a convenient, cost -effective modality exists to recognize and initiate early treatment is so readily available, in the form of mobile teleradiology services, this should be considered an important tool in the early recognition of the HRRP monitored diseases, and action taken to implement these novel approaches.. In this new environment, of ACA mediated Medicare reforms, such as the HRRP, the new guidelines poses a substantial financial penalty. Ideally, these provisions will lead to not only decreased rates of readmission, but an overall decrease in morbidity and mortality, lives saved.
With the enactment of the Affordable Care Act provisions were made with the goal of universal health coverage and ultimately, improved health and well being of our nation’s citizenry. Special provisions were made to include Medicare reforms through a caudry of special programs, one we have touched on here, the Hospital Readmission Reduction Program, aimed at improving health outcomes for seniors and securing the Medicare Program through a series of initiatives which will generate billions of dollars back into the program. The law also includes initiatives to improve quality-based medical treatment as well as promote new models of healthcare delivery, reduce waste and modernize our healthcare system. While it is still too early to tell, data compiled on specific initiatives, could show progress in improving outcomes on specific common illnesses, such as the diseases we have discussed in this piece. Further, data will follow and allow us further to evaluate the degree to which progress is being made and areas which require further study or improvement, to determine overall, how we are doing as a nation in achieving the lofty goals inspired by the Affordable Care Act. The ACA tasked our healthcare system with providing evidence-based, novel strategies to improve healthcare outcomes.. The services provided by groups such as Vesta are innovative, cost-effective and subject to multiple levels of quality assurance initiatives that provide the transparency and compliance data required in this new healthcare landscape.








 Studies suggest
Studies suggest