Just before October 2022–Breast Cancer Awareness Month–Katie Couric publicly revealed that her mammogram a few months earlier had alerted her doctors that she needed further medical tests, and this testing led to her diagnosis of breast cancer. Fortunately, she and her doctors had caught her cancer early on and had time to act on the diagnosis.
Katie’s career as a successful news anchor brought attention to the reality that breast cancer can happen to anyone. She felt her bold announcement of the disease might help reduce new cases of invasive breast cancer. That was her objective with many interviews and publicity on television, in magazines, and other media.
Campaigns are More Important This Year
During the pandemic, many women went without seeing their physicians or getting mammograms. The Journal of American Medical Association estimates breast cancer screenings have reduced by 6% in the past two years. With breast cancer causing worldwide deaths of over 685,000 in 2020, early detection with mammograms is essential.
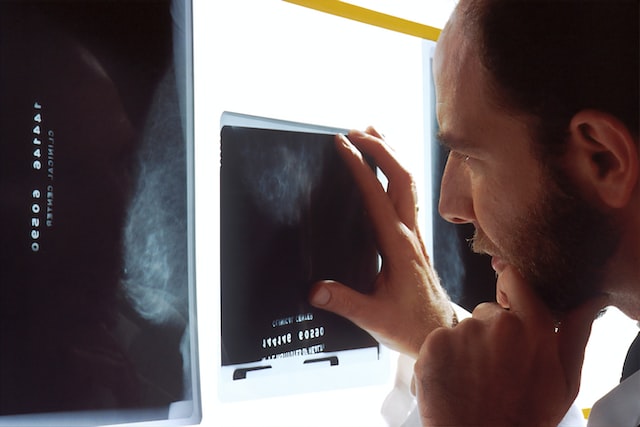
Mammograms are just an X-ray to detect abnormalities in a woman’s breast tissue; however, these images have found cancers up to 3 years before a patient can feel any lumps in the breast tissue.
Just about everyone is aware of the importance of mammograms in the fight against breast cancer, but many do not follow through with the process of making and showing up for mammogram appointments. Creative campaigns to motivate women to follow through with their health care can save many lives.
Campaign Strategies
The Centers for Disease Control and Prevention has issued a digital media toolkit to focus constructive messages to the public about Breast Cancer Awareness. The toolkit is structured to empower women to take control of their health and do what they must do for an early diagnosis of breast cancer.

Every campaign initiated by organizations, workplaces, and individuals should emphasize routine mammograms because they can be the key to saving a woman’s life. The mammogram is an easy exam, but it’s equally easy to forget or delay.
During October, many clinics or private practitioners offer free mammograms to low-income or uninsured women between the ages of 40 and 64. Individuals can help these organizations get the word out to the public by volunteering to help spread the word. The word free is a very effective campaign strategy.
The Susan G. Komen Foundation has multiple races across the country to bring awareness and financial support for breast cancer awareness. Their strategy is to create an event for the participants to go out and raise money for their cause. Their strategy is power in numbers, and the walks have been very successful for the foundation.
Employers can get involved with campaigns for their employees as well. Workplace wellness plans have partnered with their insurance companies to offer personal assessments for their employees, bring in mobile mammography vans, and promote educational information for the women in their workplace.
Anyone can have a successful campaign to bring awareness to breast cancer prevention and early detection. Finding strategies that work for each individual, community, and culture can sometimes be challenging but worth the effort. After all, it is about getting the word out and, more importantly, saving lives.
Read More Mammograms with Teleradiology
By partnering with a teleradiology company like Vesta, you will be able to get more mammogram screenings done since we can handle the interpretations for you, days, nights and weekends. Want to learn more about how we integrate with your workflow? Contact us now for a free quote and overview: 1-877-55-VESTA.