Every year, hospitals experience an influx of patients during winter due to respiratory illnesses, falls, and accidents. However, with the ongoing pandemic, the winter season brings extra challenges for the medical staff.
Preparing ahead is crucial to ensure that hospitals can cope with the surge in the winter season.
What to Expect
The winter season often increases respiratory illnesses such as pneumonia and bronchitis. Hospital admissions for these conditions can increase by up to 25% during winter. Medical staff should expect to see more patients with respiratory illnesses in 2023/2024.
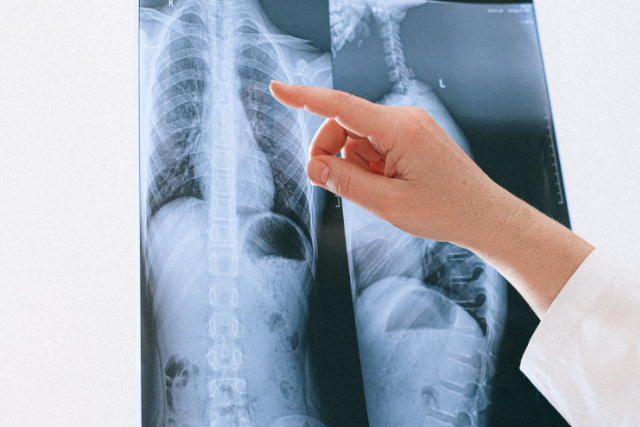
Imaging procedures such as X-rays and CT scans can help to diagnose and monitor these conditions. Therefore, hospitals should ensure enough imaging technicians, equipment, and supplies.
Hospitals can also expect more patients with falls and accidents. Icy roads and pavements can cause slips, trips, and falls, leading to broken bones and head injuries.

Imaging procedures such as X-rays and MRI scans can help to diagnose fractures and internal injuries. Therefore, hospitals should ensure that they have enough imaging equipment to diagnose and monitor these injuries.
They should also provide an imaging safety committee to promote safety in the imaging department.
With the ongoing pandemic, hospitals should expect a surge in COVID-19 patients during the winter season. The increase in COVID-19 cases will put additional pressure on hospital resources.
Imaging procedures such as chest X-rays and CT scans can help to diagnose and monitor COVID-19 patients. Therefore, hospitals should ensure enough imaging equipment to diagnose and monitor COVID-19 patients.
They should also have policies and procedures to protect staff and patients from infection.
How to Prepare
The winter season not only brings a surge in patients but also a surge in demand for medical staff. Hospitals should expect medical staff shortages to increase during the winter months due to staff illness, vacation time, and extra medical staff needed to manage the surge.
Therefore, hospitals should consider hiring temporary medical staff during winter to cope with the increased demand. They should also provide ongoing training for new and temporary staff, including imaging technicians.
Vesta Teleradiology to fill in Gaps and Radiologist Shortages
In conclusion, the winter influx of patients can be challenging for hospitals, especially with the ongoing pandemic. Hospitals should prepare to cope with the patient surge and medical staff shortages.
Imaging procedures can help to diagnose and monitor respiratory illnesses, falls and accidents, and COVID-19 patients. Therefore, hospitals should ensure that they have enough imaging equipment, technicians and of course radiologists for interpretations. Vesta Teleradiology provides US Board Certified radiologists who will work with you day and night, 24/7.
They should also have policies and procedures to protect staff and patients from infection. By preparing ahead, hospitals can ensure that they provide the best possible care for their patients during winter.



















 Sources:
Sources: