Urgent care facility service use has increased substantially in recent years. Urgent care services’ popularity has provided conveniences and cost reductions of medical care needs.
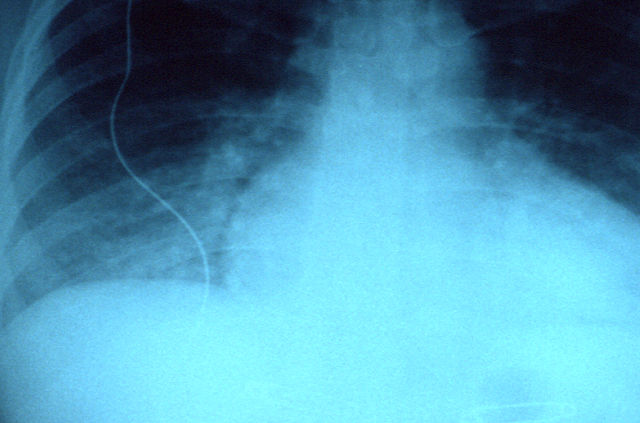
When a patient enters an urgent care facility, the treating provider determines if radiology services will aid in the diagnosis and treatment plan for the patient. A medical assistant or radiology technician will then use the equipment to produce the radiological images.
Once the technician creates the radiological images, the treating provider will view and diagnose or send the images to an expert at the teleradiology service contracted with the facility.
Broken bones are not the only reason an urgent care patient may access care at a convenient, local care medical facility. Patients arrive at the facilities for possible strokes, abdominal obstructions, complex pediatric ailments, and other health conditions. Expert radiological assessments can be crucial in practical and immediate treatment.
When a patient who needs radiology services accesses an urgent care facility, fast and professional analysis is essential for effective treatment.
Teleradiology services have fit in nicely with the goals and objectives of the urgent care facilities for various reasons. Not all patients accessing urgent care need radiology services. Although the service can be life-saving if required, the low rate of use does not warrant the staffing of a full-time radiologist at each facility.
Contracting radiology services for these facilities allows a full-time expert to be available at all times, and these cost savings of a full-time employee are significant.
Teleradiology services allow a physician to access experts anywhere in the country. The pool of providers is not only available at any time, but a radiology expert’s conclusive reports can be sent securely and quickly.

If the treating physician has questions about any findings, the radiology expert is easy to reach. This convenience is also possible if the patient or physician requests a second opinion on the results.
With the convenience of radiological expertise availability, urgent care providers can also reduce their professional liability. Providers creating treatment plans for various injuries and symptoms can benefit an urgent care facility contracted with a teleradiological service. Many teleradiology service companies provide a resource for physician consultation.
Choosing a Teleradiology Company for Your Hospital
Contracting with a teleradiology service can reduce liability for the urgent care facility while increasing and maintaining an excellent public reputation.
The medical care profession has changed drastically over the years, and so have the healthcare consumers. Consumers expect better service, insurance companies expect more conservative costs, and treating physicians need fast results with less liability.
Teleradiology fits nicely into the niche of urgent care facilities because it fits all the criteria of a rapidly changing medical system structure. Teleradiology can be a crucial component for a clinic to provide an ideal service of expert care at an exceptional value.
Teleradiology: Best Providers
Vesta has been providing expert radiology services for over 15 years. We use state of the art technology to streamline your workflow and provide stat readings whenever required. Whether you operate an urgent care center or a private practice our US Board Certified Radiologists are here to help you literally 24×7, even on weekends and nights.

Please contact us for a custom proposal and a complimentary overview of our services and technology.