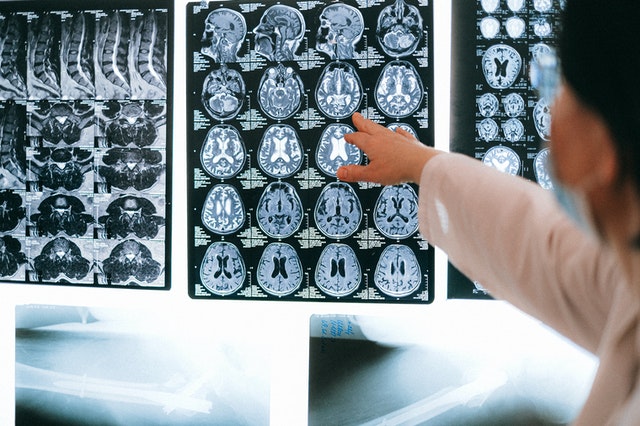
The emergence of ChatGPT in the medical field, particularly in radiology, has generated a mix of excitement and concern about its role. But is it accurate enough to put into use? Can we trust artificial intelligence (AI) with the health of our patients?
How Could ChatGPT be Used?
An article in Diagnostic and Interventional Imaging discusses various ways in which radiologists can leverage ChatGPT. It highlights applications for clinical radiologists, such as implementing ChatGPT as a chatbot for patient inquiries, supporting clinical decision-making with information and analysis assistance, and enhancing patient communication and follow-up care by simplifying radiology reports and crafting tailored recommendations. Academic radiologists can benefit from ChatGPT by receiving suggestions for impactful research article titles, assistance with structuring and formatting academic papers, and help in formatting citations for bibliographies. The article emphasizes that the best use of ChatGPT in radiology depends on individual needs and goals, potentially paving the way for a more intelligent future in the field. It notes that while ChatGPT offers valuable support, it’s crucial to fact-check its answers and review its output to ensure accuracy and relevance.
What Radiologists Have to Say
In RSNA’s article, The Good, the Bad and the Ugly of Using ChatGPT, various radiologists give their opinions on the use of this AI. Dr. Som Biswas, who published an article in Radiology entirely written by ChatGPT, believes that its potential benefits in reducing the workload and improving efficiency in radiology outweigh its limitations, which could be especially valuable in addressing the growing demand for medical imaging and reports in the face of a radiologist shortage.
Yiqiu Shen, MS, a researcher at New York University’s Center for Data Science, remarked, “In general, it’s ok to use ChatGPT as a language aid or to provide a template, but it’s dangerous to rely on ChatGPT to make a clinical decision.”
Urologic Imaging and AI: A Study
A study published in Current Problems in Diagnostic Radiology compared the performance of OpenAI’s ChatGPT and Google Bard in suggesting appropriate urologic imaging methods based on American College of Radiology (ACR) criteria. Both chatbots demonstrated an appropriate imaging modality rate of over 60%, with no significant difference between them in the proportion of correct imaging modality selected. However, the researchers noted that both chatbots lacked consistent accuracy and further development is needed for clinical implementation. The study found that while the chatbots were not entirely consistent in their responses, they hold promise in assisting healthcare providers in determining the best imaging modality, potentially improving clinical workflows in the future. ChatGPT provided shorter responses and had a slightly longer response time compared to Bard, which was faster but struggled with determining appropriate imaging modalities in a few scenarios.
Vesta: A Tech-Forward Company
Vesta Teleradiology looks forward to a future integrating AI with medicine. Click here to read more about Vesta Teleradiology Partners with MIT for AI Research
Sources:
radiologybusiness.com
rsna.org
Auntminnie.com
openai.com












 Sources:
Sources: