Today’s smart hospital is not just a paperless organization with digitized charting. Although being digitized is an excellent start to a smart hospital, the process is much more advanced.
The goal of a smart hospital is better patient care while streamlining operational efficiency and costs. Three essential layers need to be addressed by a hospital to achieve the classification of a “smart” facility.
Step 1–Operations
Even though all hospitals gather information about their patients, operations, and management, a smart hospital takes gathering data to a different level.
In a smart hospital, analytic systems and software integrate all the information utilized by doctors, nurses, facility personnel, and administrators. A desktop, smartphone, or handheld device can access this information, resulting in faster, more efficient decision-making by key people.
With automated systems, the management of staff, pharmaceuticals, supplies, consumables inventory, assets, equipment, patients, and even visitors is controllable by the appropriate hospital teams. The process is cost-saving and efficient for the hospital and the patient.
To achieve these network-based services, hospitals with a large traffic volume and frequent environmental changes best utilize 5G or Wi-Fi 6 technology which is a step up for most hospital internet access.
Step 2–Clinical Tasks
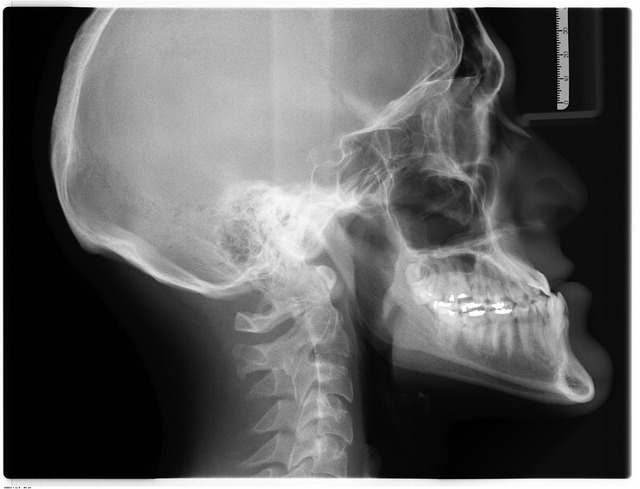
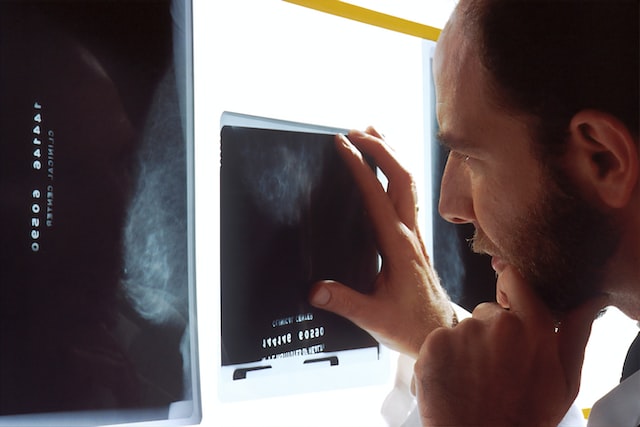
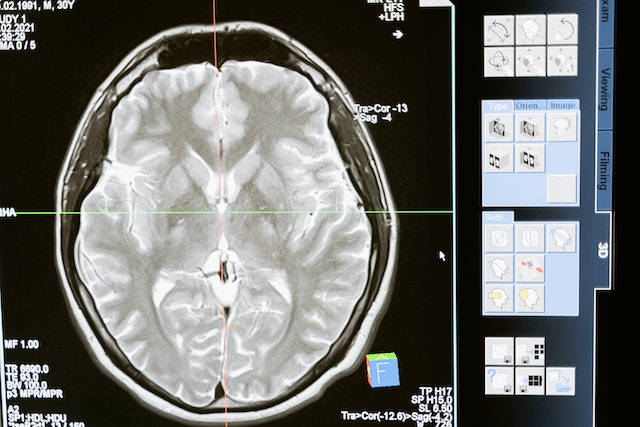
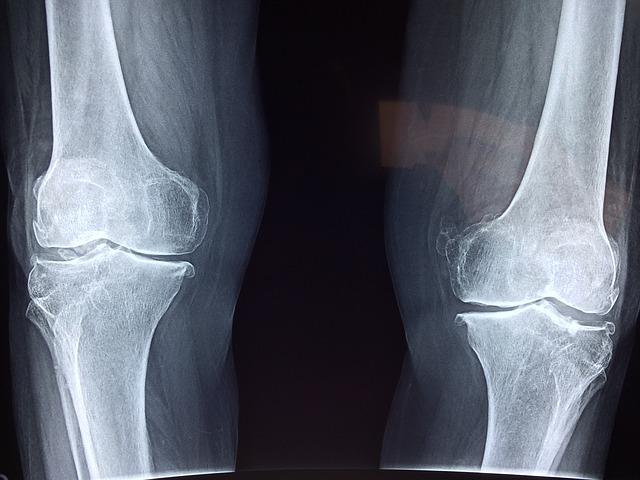
The doctors’ and nurses’ efficiency depends on communication with departments like critical care, surgical, and technical (lab and X-ray) services.
A smart hospital improves patient outcomes by utilizing remote monitoring tools. Medical professionals can immediately monitor a patient’s vital signs, steps, heart rates, allergies, and lab results. The added communication also allows more patient input about likes, dislikes, and comfort zones. Smart hospitals will also utilize teleradiology services like Vesta in order to process more imaging interpretations remotely and efficiently.
INSIDE CANADA’S FIRST SMART HOSPITAL
Step 3-Patient Care
A patient’s room is very different within a smart hospital. A patient can access help through voice-based interactive devices to dim the lights, call a nurse, request pain medication, or make phone calls to loved ones—no more worries about a dropped call button on the floor.
The smart hospital design focuses on enhancing the healing process for faster recoveries by featuring open spaces and gardens. Children can also have specially designed areas for their comfort.
Caring robots in hospitals are providing added support in the facilities. Smart hospitals have programmed robots to perform surgeries; provide dementia care for the elderly; provide biofeedback for patient anxiety; transport supplies, blood, medication, meals, and garbage.

Hospitals have also programmed robots to provide care in quarantine isolation booths or entertain hospitalized children for a more positive emotional experience.
The Future
The future of smart hospital strategies is endless. The hospital environment and opportunities will continue to expand for the cost and convenience benefits of the hospital operations and its patients. The hospital will be able to extend most of the “smart” gifts to the patient’s home.
Patients will be able to take home smartwatches and other monitoring equipment for continued hospital care. More utilization of mobile monitoring equipment will allow the hospital to operate as intended–for emergencies, surgeries, and intensive care units–and will enable the patient to recover safely in the comfort of their home. And even more exciting is the future use of Artificial Intelligence to further enhance the benefits of the smart hospital.