The role of the radiologist has changed over recent years. The health care world once thought of these professionals as sitting in a dark room interpreting imaging data and writing reports.
Today, diagnostic imaging is used by physicians more, and the radiologist’s role has become more centrally involved with patient care. There are opportunities to connect to the patients during the diagnostic imaging process that other health care providers don’t have.
Patient comfort during any healthcare procedure provides a series of activities that gain trust and provide emotional security in the process. Diagnosticians’ communication with their patients must convey that the staff is dependable, empathetic, and knowledgeable.
Environment
When patients first arrive for their appointment, they may be apprehensive and anxious about what their diagnostic imaging may reveal about their health and future.
The waiting room is where the patients not only wait for their appointment, but it is a place where they can talk with family members. Giving the seating lots of space allows areas with quiet corners for people to speak and express anxieties they may be experiencing.
A waiting room with plants, windows, and possibly waterfalls and nature scenes provides space for relaxation, gathering thoughts, and exploring possible questions about the procedure.
Physical Comfort
Diagnosticians performing a baseline assessment of the patient’s pain levels before, during, and after any invasive procedure is essential. It is also necessary to educate staff on any pain control protocols.
Patients appreciate simple office organization like short wait times in scheduling to minimize stress. Patients also appreciate comfortable procedure gowns, comfortable room temperatures, and warm blankets, along with sheets and pillows covering the procedure tables.
By reducing the technology sounds like beepers and overhead speakers, patients can have an easier time relaxing.
Communication
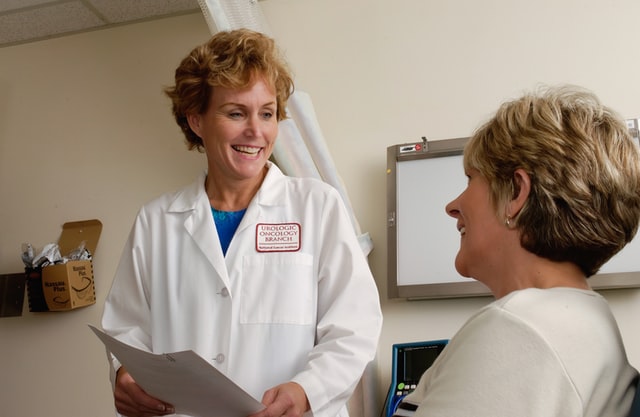
Effective communication can begin with the diagnostician partnering with the patient and their families to ensure that needs and preferences are being met. By involving the patient and their family, decision-making becomes more straightforward and more confident.
Patient-centered communication skills encourage the patient to talk about psychosocial issues that may affect their health or procedures. Through this communication process, the diagnostician can respect their patient’s requests and values and address or provide counseling and resources for patient support.

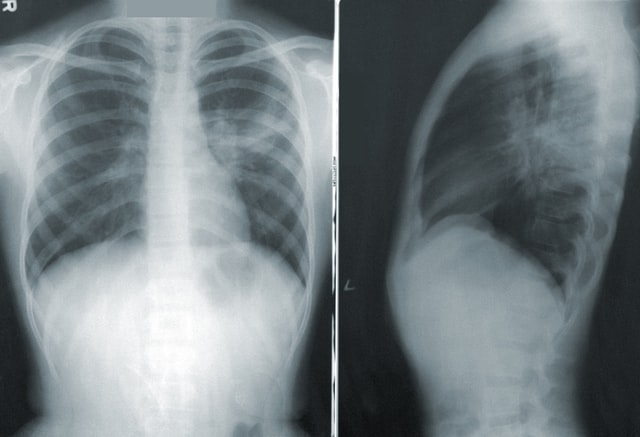
The top priority in the patient and health care provider relationship is maintaining an open and honest relationship. Diagnosticians can be sure the patient understands the procedures and the results of the processes by spending time, and using any tools that can assist is most valuable.
Tools like questionnaires, pamphlets, and visual aids can help the health care provider explain the benefits, risks, procedures, and processes or what is happening with the patient’s health.
Paying attention to the patient’s emotional concerns and using their own words when encouraging them to express themselves builds their trust with their health care providers.
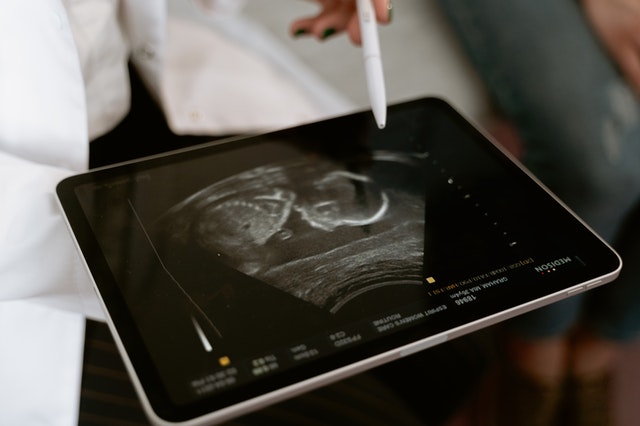
Imaging diagnosticians can use the time spent with the patient as teachable moments. For example, during mammography appointments, staff can inform and educate patients about the importance of colon screening and bone density tests.
It is also crucial for health care providers to practice restraint and allow quiet time for their patients. There is sometimes a tremendous amount of information to process, and it takes time for patients to deal with their feelings and formulate essential questions they may have.
The importance of diagnostic imaging will continue to expand in the health care field. Advancements in cancer treatments, diagnoses, and disease prevention rely heavily on the professionalism of diagnostic imaging.
These health care professionals can experience positive relationships and trust with their patients by providing needed emotional support and conveying a genuine sense of caring.
Vesta Teleradiology wants to help you make your patients’ experience as streamlined as possible. That’s why we offer tools and customizable reports that work WITH your current workflow. We also offer 24x7x365 radiology reading services so your radiologists can have a better work life balance.











 Studies suggest
Studies suggest