Medical science makes incredible strides every year, finding new ways to heal the sick and injured. One of the most exciting of these new frontiers is ultrasound technology.
With its ability to safely and painlessly penetrate the human body, scientists and doctors are discovering new possibilities in diagnosing and treating conditions that previously required more invasive procedures.
Ultrasound in Cancer Treatment
In cancer treatment, chemotherapy often comes with various unpleasant side effects. But new research has shown that ultrasound technology can enhance chemotherapy effectiveness, sometimes even reducing the dosage of the drugs required.
Ultrasound can also help increase the uptake of cancer drugs into tumors, making their delivery more targeted and efficient.
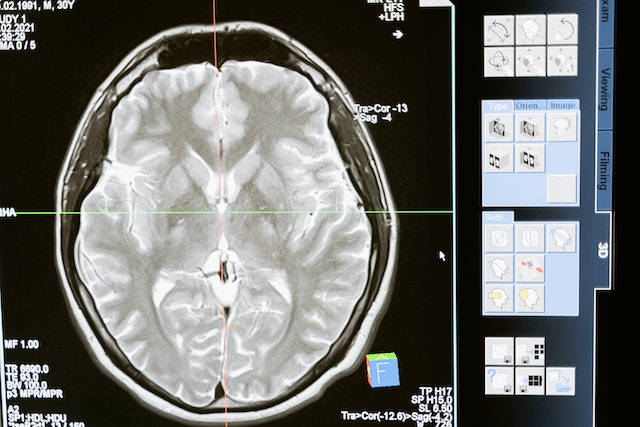
Ultrasound and Alzheimer’s Disease
Alzheimer’s disease is one of the most heartbreaking conditions facing our aging population, and while there is no cure for it, there is hope for better treatment.

Recent research has discovered the possibility of using ultrasound to break up the plaques that form in the brains of Alzheimer’s patients, reducing the inflammation and damage that cause the disease. Research in this field is still in its early stages, but the possibility of a breakthrough treatment in the years to come is an exciting prospect.
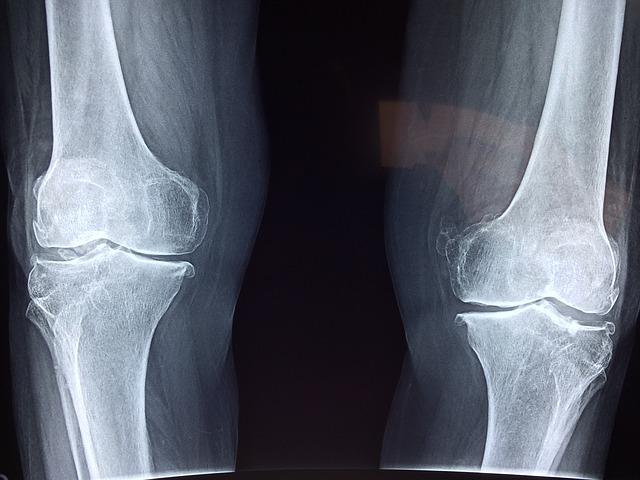
Ultrasound Diagnostics
Of course, one of the primary uses of ultrasound in medicine is as a diagnostic tool. However, new studies are refining and expanding the possibilities of what ultrasound can detect.
For example, technicians now use ultrasound to locate and diagnose skin cancers and traditional mammography for breast cancer screening. Ultrasound also offers a non-invasive way to examine the heart and blood vessels in incredible detail, giving doctors a better understanding of the mechanisms of cardiovascular disease.
Ultrasound and Pain Management
In addition to being an incredible diagnostic tool, patients can use ultrasound to manage pain.
Ultrasound-guided nerve block injections can relieve patients suffering from chronic pain without the side effects of prolonged medication use. Studies are ongoing to refine this technique and expand its benefits beyond chronic pain.
Other Applications of Ultrasound
The research and innovation happening in ultrasound are constantly expanding their possibilities.
For example, researchers are exploring ultrasound technology to treat kidney stones, sometimes allowing for less invasive procedures than traditional surgery.
They are also investigating ultrasound for use in regenerative medicine and even to monitor blood glucose levels in diabetic patients non-invasively.
The possibilities of ultrasound technology seem almost limitless, with new studies constantly uncovering ways to use this powerful tool for medical treatment and research.
From cancer treatment to pain management, diagnostics to disease prevention, ultrasound is a field that promises to revolutionize the face of medicine in the years to come. We can only look forward with enthusiasm and hope for what discoveries may come on this exciting frontier.
Teleradiology in Conjunction with Ultrasound
When you think about the role a teleradiology company like Vesta plays with healthcare providers, you might envision that the radiologists deal only with x-rays and MRI scans. We also work closely with hospitals for ultrasound readings, too. If you’re seeking an extra hand for preliminary and final ultrasound interpretations, please reach out to us today. We can handle any volume, large or small.