- Attrition (radiologists leaving clinical practice) rose from 1.1% in 2014 to 2.5% in 2022 in a national analysis of 41,432 radiologists.
- Subspecialists were more likely to exit than generalists (adjusted OR 1.37), which can widen gaps in high-demand service lines.
- Rural-linked practices and nonacademic settings showed higher attrition signals—often where backup coverage is hardest to source.
What the new AJR study found (and why leaders should care)
A 2026 AJR study analyzed CMS National Downloadable Files (2014–2022) and linked them with claims datasets to identify when radiologists were no longer clinically active—i.e., attrition. The topline result is simple but operationally huge: radiologist attrition increased steadily over the period, reaching 2.5% by 2022 (unadjusted).
For imaging leaders, attrition isn’t just a workforce statistic. It shows up as:
- Harder scheduling and more uncovered shifts
- More frequent “thin coverage” windows (nights/weekends/holidays)
- Longer turnaround time risk when volumes surge
- Greater dependence on a smaller bench of subspecialty readers
The subspecialty problem: “more demand, fewer experts”
The study’s most concerning signal for many hospitals is who is leaving. After adjusting for multiple factors, subspecialists had higher odds of exiting than generalists (OR 1.37).
Why this matters: subspecialty reads aren’t evenly interchangeable. When the local bench thins, the first pain points tend to be:
- Neuro (stroke pathways, head/neck CTA/CTP, complex MRI)
- MSK (trauma MRI, occult fractures, postop complications)
- Body (oncology staging, complex abdomen/pelvis CT/MR)
- Chest/cardiothoracic (PE, ILD, oncology follow-up, CTA)
In practical terms, a smaller share of subspecialists can lead to more “general coverage” during peak times—and that often creates inconsistency in reporting, more clarification calls, and slower decision loops.
Attrition isn’t evenly distributed across settings
The AJR analysis also found higher adjusted odds of attrition for:
- Nonacademic vs academic radiologists (OR 1.34)
- Radiologists in practices with at least one rural site (OR 1.16)
That matters because rural and community facilities often have:
- smaller groups,
- fewer redundant subspecialists,
- limited ability to recruit quickly,
- and higher sensitivity to coverage gaps (one vacancy can shift everything).
Separately, the ACR’s workforce update highlights consolidation and changing practice structures as part of the broader environment imaging leaders are navigating.
 What hospitals can do now (short-term, operations-first)
What hospitals can do now (short-term, operations-first)
A 2024 AJR paper on short-term strategies argues that no single fix solves supply vs demand—so leaders should combine workflow efficiency moves with coverage planning.
A hospital-ready approach often looks like this:
1) Protect “minimum viable coverage”
Define what must be covered to keep patient flow safe (ED CT, stroke imaging, critical inpatient STATs, weekend lists). Put it in writing so you can activate a plan quickly when staffing flexes.
2) Separate urgency tiers
If everything is “STAT,” nothing is. Clear categories + escalation paths reduce noise and protect turnaround time for truly time-sensitive studies.
3) Build redundancy for the riskiest windows
Overnights and weekends are where small cracks become big delays. Redundancy can be internal (cross-coverage) or external (a vetted partner).
4) Treat subspecialty access as a service line
If neuro/MSK/body reads are crucial to downstream programs (stroke center, ortho service, oncology), plan coverage like a core capability—not a nice-to-have.
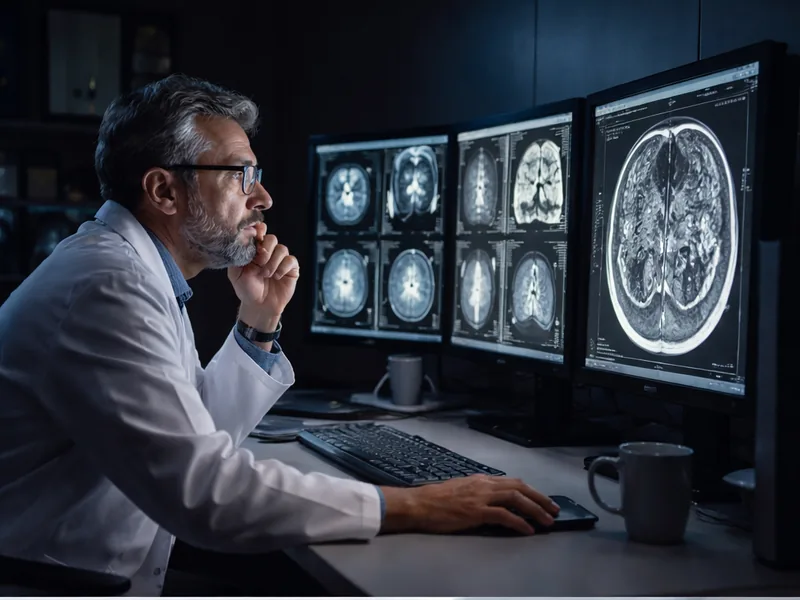
Where Vesta Teleradiology fits
Vesta supports hospitals and imaging centers with reliable coverage and subspecialty-capable interpretation to reduce the operational risk that comes when local staffing gets stretched. When attrition disproportionately affects subspecialists, a flexible teleradiology partner can help you:
- maintain consistent subspecialty reads,
- protect night/weekend coverage,
- stabilize turnaround time during spikes,
- and keep clinical teams moving from imaging to decision without delay.
Learn more at vestarad.com.

 3) Smooth scheduling around your true capacity
3) Smooth scheduling around your true capacity


 Why this RSNA prize matters for teams—not just individuals
Why this RSNA prize matters for teams—not just individuals
 New trial evidence favors MRI and contrast-enhanced mammography
New trial evidence favors MRI and contrast-enhanced mammography
 Growing Market and Adoption
Growing Market and Adoption