Key Takeaways
AI shifted from pilot projects to real workflow infrastructure—with more focus on governance, validation, and safety in daily operations.
Photon-counting CT moved closer to mainstream adoption, strengthening the business case for next-gen CT planning and protocol upgrades.
Reimbursement and policy pressure stayed intense, keeping budgeting, contracting, and service-line ROI under a microscope.
Prior authorization and imaging appropriateness remained major throughput challenges, impacting scheduling, patient access, and operational efficiency.
Cybersecurity and downtime readiness became core imaging priorities, as ransomware and system disruptions increasingly threaten continuity of interpretation.
Radiology didn’t have a single “one story” year—it had a “many small shifts became operational reality” year. In 2025, diagnostic imaging leaders saw AI move from pilots into production workflows, next-gen CT mature from promise to procurement conversations, reimbursement pressures intensify, and cybersecurity become inseparable from patient care. Meanwhile, staffing strain and consolidation continued to reshape how coverage is delivered.
Below is a practical wrap-up of the biggest breakout themes from 2025—and what they signal for 2026 planning.
1) AI moved from point solutions to regulated, workflow-embedded infrastructure
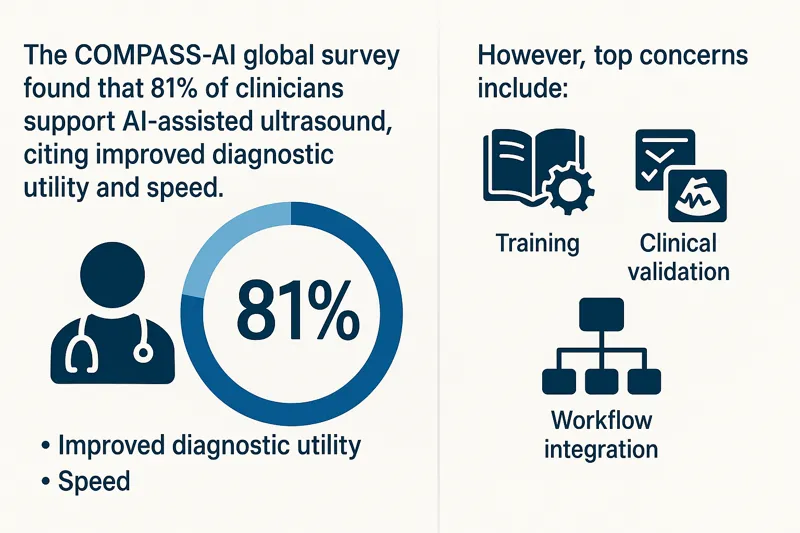
If 2023–2024 was the era of “AI can detect X,” 2025 was the era of “AI has to behave safely inside real clinical systems.” Regulatory claritya and operational expectations became the story as much as the algorithms themselves. RSNA’s coverage highlighted how the FDA has been articulating pathways and challenges for AI-enabled radiology devices—making governance, validation, monitoring, and safety considerations a board-level topic, not just an R&D conversation. Daily Bulletin
At the same time, 2025’s conversation broadened from task-specific tools to foundation models and multimodal systems (images + text) that could impact triage, reporting support, and quality workflows—while also raising new risks around bias, generalizability, and clinical readiness. DirJournal
Operational takeaway for imaging leaders: AI value in 2025 increasingly depended on integration (PACS/RIS/reporting), change management, and clear accountability—especially as adoption expands and expectations shift from novelty to measurable outcomes. The Washington Post
2) Photon-counting CT stepped into the “real adoption” phase
Photon-counting CT (PCCT) wasn’t framed as a future curiosity this year—it showed up as a maturing platform with expanding clinical evidence and increasing operational readiness. RSNA 2025 coverage specifically called out how PCCT is taking center stage as the next CT evolution. Applied Radiology
 Across 2025 literature and trade coverage, the narrative tightened around what administrators care about: clearer visualization and characterization, potential dose efficiencies, and broader specialty applications as the evidence base grows. ScienceDirect
Across 2025 literature and trade coverage, the narrative tightened around what administrators care about: clearer visualization and characterization, potential dose efficiencies, and broader specialty applications as the evidence base grows. ScienceDirect
Operational takeaway: If you’re building 3–5 year replacement plans, 2025 made PCCT a serious line item conversation—especially for high-volume sites where incremental image quality and protocol optimization can compound into throughput, repeat-scan reduction, and clinician confidence.
3) Payment pressure stayed relentless—and policy debates sharpened
For many departments, 2025 felt like a year of doing more with less. The 2025 Medicare Physician Fee Schedule (MPFS) final rule remained a major planning input for imaging groups and hospital finance teams, with ACR publishing a detailed imaging-focused summary of provisions and QPP updates. American College of Radiology
At the end of the year, broader Medicare payment policy debates also made headlines—reinforcing that specialty payment and “efficiency” assumptions are likely to stay politically active topics heading into 2026. Axios
Operational takeaway: Contracting, service line budgeting, and modality ROI assumptions increasingly need “policy sensitivity” built in—especially for outpatient imaging strategy and subspecialty coverage models.
4) Utilization management: prior auth and “right test, right patient” stayed in focus
Utilization controls continued to evolve. CMS prior authorization programs for certain outpatient services remain part of the broader backdrop of controlling unnecessary volume. CMS And late-2025 headlines underscored expanding demonstrations tied to prior authorization in additional settings, which imaging leaders often experience downstream as scheduling friction, referral leakage, or delayed care. Kiplinger
On the imaging appropriateness front, the Medicare AUC program remains a major framework (even as implementation timelines and mechanisms continue to be debated). CMS In 2025, ACR also publicly backed federal legislation (the ROOT Act) positioned as a way to revitalize Medicare imaging appropriateness workflows. American College of Radiology
Operational takeaway: Expect “appropriateness” and “utilization proof” to keep rising as operational requirements—meaning your radiology operation will benefit from tighter ordering communication loops, smarter triage, and documentation hygiene.
5) Breast imaging compliance stayed operationally important—density language included
Breast density notification requirements became routine compliance work after enforcement of MQSA’s amended regulations began in 2024, and 2025 was about living with the operational realities: consistent report language, patient communication workflows, and inspection readiness. U.S. Food and Drug Administration
Notably, 2025 also saw attention on density reporting language options under MQSA—an example of how “small wording changes” can have major downstream effects in templates, patient letters, and audit processes. DenseBreast-info, Inc.
Operational takeaway: Standardization wins here—clear templates, audit trails, and staff training reduce risk while improving patient communication consistency.
6) Workforce strain and burnout remained the constant—and coverage models kept shifting
Radiology’s capacity crunch persisted in 2025. ACR continued to flag ongoing workforce shortages amid rising imaging demand, while national physician burnout tracking suggested improvement from prior peaks but still elevated rates that affect retention and coverage reliability.
Operational takeaway: The “coverage plan” is now a strategic asset. Departments that treat coverage as a system (subspecialty access, peak-demand flex, nights/weekends/holidays, overflow protection, and consistent turnaround governance) are better positioned for 2026.
7) Cybersecurity became inseparable from imaging operations
Cyber risk is no longer “IT’s problem”—it’s a continuity-of-care risk, especially for imaging organizations that depend on always-on networks and data flow. In 2025, radiology-specific alerts and incidents reinforced how real the threat landscape is, from FBI-linked warnings about ransomware targeting healthcare entities to major breach reporting involving large imaging providers. Radiology Business
 Operational takeaway: Imaging leaders should be asking: Do we have downtime playbooks? How resilient is PACS access? How are third-party integrations governed? How do we preserve interpretation continuity if local systems are disrupted?
Operational takeaway: Imaging leaders should be asking: Do we have downtime playbooks? How resilient is PACS access? How are third-party integrations governed? How do we preserve interpretation continuity if local systems are disrupted?
A 2026-ready checklist for imaging leaders
Here’s what 2025’s headlines suggest you prioritize next:
- AI governance that’s operational, not theoretical: validation, monitoring, and workflow accountability.
- Modern CT strategy: map where photon-counting CT could change protocols, dose strategy, and long-term equipment planning. Applied Radiology
- Payment + policy resilience: bake MPFS sensitivity into budgets and service line forecasts.
- Utilization friction planning: anticipate prior-auth expansion impacts on scheduling and throughput.
- Compliance consistency in breast imaging: templates, audits, and MQSA-ready workflows.
- Coverage strategy as a system: subspecialty access + surge/overflow + nights/weekends/holidays planning.
- Cyber continuity: imaging downtime workflows and vendor access governance.
Where Vesta Teleradiology fits in a “do more with less” reality
For hospitals and imaging centers, one of the most immediate ways to de-risk 2026 is to strengthen coverage—especially when staffing shortages collide with growing imaging demand. Vesta Teleradiology supports facilities with 24/7/365 coverage (including nights, weekends, and holidays) and subspecialty radiology interpretations designed to integrate with your existing technology and workflows.
If you’re planning for 2026 coverage resilience—overflow protection, consistent turnaround times, or expanded subspecialty reads—you can request a quote or schedule a test run here.





 Why It Matters for Facilities and Radiology Teams
Why It Matters for Facilities and Radiology Teams
 Growing Market and Adoption
Growing Market and Adoption



 This extension is part of CMS’s ongoing efforts to maintain flexibility in healthcare delivery, particularly in response to the challenges posed by the COVID-19 pandemic. Initially introduced in 2020, the virtual supervision policy has been extended multiple times, reflecting its effectiveness in enhancing access to care, especially in rural and underserved areas.
This extension is part of CMS’s ongoing efforts to maintain flexibility in healthcare delivery, particularly in response to the challenges posed by the COVID-19 pandemic. Initially introduced in 2020, the virtual supervision policy has been extended multiple times, reflecting its effectiveness in enhancing access to care, especially in rural and underserved areas.