If you’ve heard colleagues mention “MRI Online,” you’ve already met Medality—the platform’s new name and broader vision for case-based radiology education and CME. Medality
Medality offers a large, searchable library of subspecialty courses and real cases designed for busy readers. The program is ACCME-accredited to provide AMA PRA Category 1 Credits™, with 700+ hours available to claim—so credits count toward common licensure, MOC, and credentialing needs. (For context on AMA PRA Category 1 Credit™ and ACCME alignment, see AMA/ACCME guidance.) American Medical Association
What makes Medality valuable in day-to-day practice
Case-based, time-efficient learning. The library is built around short, expert-led “microlearning” lessons you can fit between cases—so you steadily upskill without disrupting coverage.
Hands-on practice with scrollable DICOMs. Medality’s case archive includes fully scrollable CT/MR studies plus brief video explanations and quizzes, helping sharpen detection speed and reporting confidence on high-yield findings.
Depth across subspecialties. From neuro and MSK to breast, cardiac, ED and beyond, courses and case sets let you target the areas your case mix demands most.
Accredited CME you’ll actually use. With 700+ AMA PRA Category 1 Credits™ available (and more added regularly), radiologists can chip away at requirements continuously rather than scrambling at renewal time.
 Why this RSNA prize matters for teams—not just individuals
Why this RSNA prize matters for teams—not just individuals
Training without lost coverage. Because lessons are on-demand and bite-sized, radiologists can learn after hours or between reads, preserving TAT while still building subspecialty confidence.
Goal-aligned upskilling. If your facility is seeing more chest pain workups, stroke alerts, or MSK injuries, you can steer readers to focused tracks and track progress via CME claims over the year.
Credentialing peace of mind. AMA PRA Category 1 Credit™ is widely accepted across hospitals and state boards, making a one-year membership a practical asset for QA plans and reappointments. (See the AMA/ACCME alignment noted above.) American Medical Association
“Is it really a $1,500 value?”
Medality’s public promos frequently reference savings or membership values up to $1,500 on premium or multi-year packages—useful as a benchmark for how substantial a full-year membership is compared with typical online CME.
Where Medality complements Vesta’s AI-enabled reading
Vesta blends subspecialty expertise with a pragmatic partner-plus-platform AI approach—dictation, PACS/VNA, and algorithm marketplaces—to deliver predictable quality and TAT. Continuous learning via Medality strengthens the skills behind that workflow, while Vesta’s operations and AI strengthen the throughput—a combined, durable path to better patient care.
How to enter the giveaway
Stop by RSNA 2025 Booth 1346 (South Hall) or email info@vestarad.com with subject “Medality CME Giveaway.” One entry per attendee; winner announced after RSNA.
About Vesta Teleradiology
Vesta provides 24/7 subspecialty reads, customizable coverage models, and seamless workflow integration for health systems, imaging centers, and rural hospitals nationwide. Learn more at vestarad.com.


 From Quantitative Imaging to Clinical Translation
From Quantitative Imaging to Clinical Translation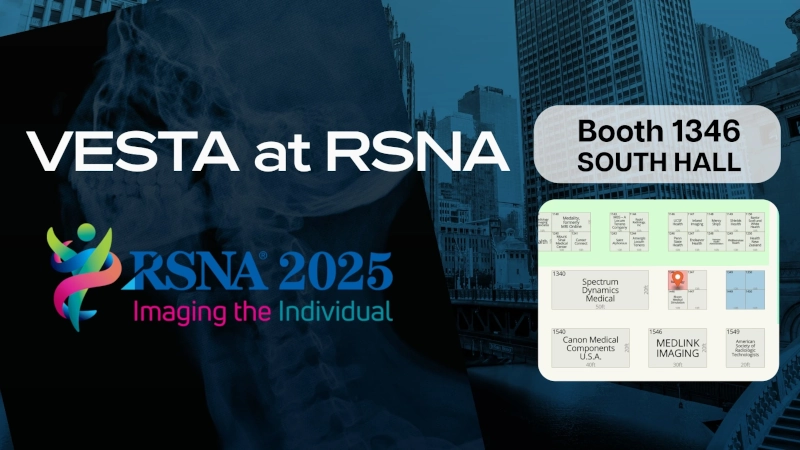


 The Rise of Digital Twins in Imaging
The Rise of Digital Twins in Imaging

 Current Impact on Patients and Healthcare Systems
Current Impact on Patients and Healthcare Systems Conclusion
Conclusion

 Sources:
Sources:
