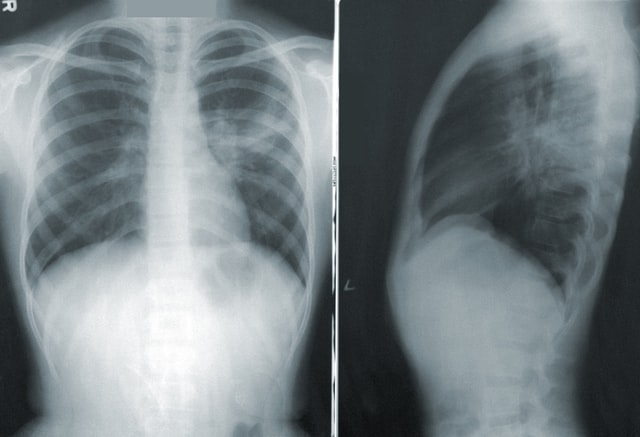
Artificial intelligence is a young field of study that has been growing exponentially as experts try to identify ways to integrate the help of machines to solve human problems. Computer systems have great potential to become facilitators in helping detect cancers and other medical conditions. It is clear that in order to advance our capabilities in patient care, we must embrace AI as it is reshaping the healthcare industry.
Massachusetts Institute of Technology (MIT) has been a pillar in research for the sciences and has been known to provide breakthroughs that benefit our lives.
MIT is in the process of developing an innovative AI Radiology application that will assist radiologists in improving the quality and speed of interpretations. Vesta Teleradiology is honored to partner with the research team in assisting with the development of this project.
Vesta has been working with various universities in supporting their needs and this partnership with MIT is inline with Vesta’s goal of helping further the research in the industry.
Each of the highly skilled Vesta radiologists will be interpreting a batch of randomly selected studies using a pre-set criteria. The interpretations are used to help enhance the algorithm and help its quality in the process. Vesta and MIT teams work very closely to make the project a success. It is through this partnership that Vesta hopes to considerably advance the field of AI in radiology and imaging.
Teleradiology Company
Vesta Teleradiology provides preliminary and final interpretations for imaging studies. They believe it is crucial to incorporate new technologies into their offerings to provide efficient solutions for healthcare providers, from hospitals to private physicians and even universities. Being at the forefront of medical advancements is part of the Vesta philosophy.
MIT is a technological innovator and is leading this effort in radiology. The contract between Vesta and MIT is sure to be one to help advance the future of medicine.
About Vesta:
Vesta exists to make life better for their healthcare facility clients and their patients through efficient teleradiology services and seamless systems integrations.