Burnout in the medical setting refers to a state of emotional, mental, and physical exhaustion experienced by healthcare professionals. It arises from chronic and excessive stress caused by demanding work environments, long hours, high patient loads, and the emotional toll of dealing with patient suffering. Symptoms of burnout include feelings of cynicism, detachment from work, reduced sense of accomplishment, and a decline in professional performance. Burnout not only impacts the well-being of medical practitioners but can also compromise patient care and safety. It also impacts staffing at all levels in healthcare, from nurses to executives.
What’s Going on Now?
Healthcare employees nationwide have initiated strikes in their efforts to secure better pay and improved staffing conditions in their employment agreements. Additionally, resident physicians are becoming increasingly engaged in labor organizing.

According to experts, these labor trends will present ongoing challenges to health systems as facilities strive to return to pre-pandemic operations while trying to control the labor costs that escalated last year. The sector is expected to face persistent staffing shortages, particularly among nurses, due to widespread burnout and increased turnover. As a result, healthcare facilities continue to rely on expensive contract labor to fill the gaps in their workforce, even as the rates of severe COVID-19 hospitalizations decline.
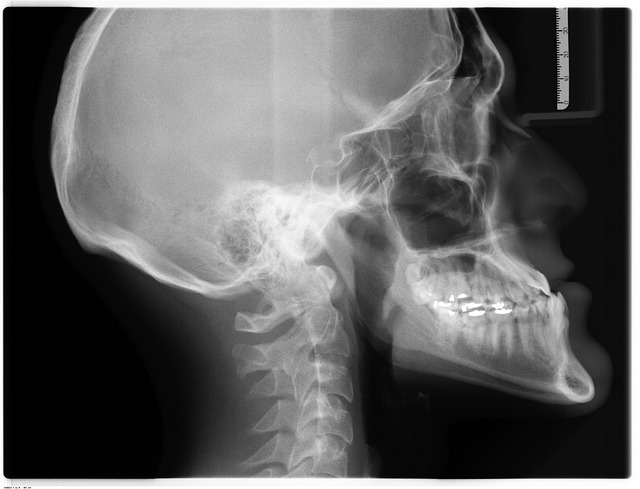
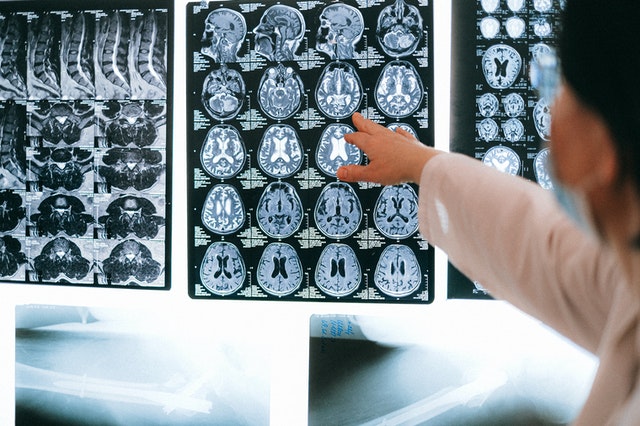
Burnout in Radiologists
The “Medscape Physician Burnout & Depression Report 2023: ‘I Cry and No One Cares'” reported that 54 percent of radiologists surveyed felt burned out. Further, just 61% of radiologists said they’re happy or very happy away from work.
Recent data published in the European Journal of Radiology presents the experiences of breast radiologists with burnout during various stages of the COVID pandemic. Surprisingly, the study reveals that, at the height of COVID, many radiologists reported improvements in five out of six common stressors, such as work pace, work-life balance, caregiving responsibilities, and financial strain. However, this relief was short-lived, as patient capacity increased again, leading to a surge in workload, backlogs of studies, and a slight increase in burnout levels compared to before the pandemic.
Addressing Staffing Shortages and Burnout
Addressing burnout is crucial to maintain a healthy healthcare workforce and ensure the delivery of high-quality medical services. Strategies like promoting work-life balance, providing support and resources for stress management, and fostering a positive and supportive work culture are essential to mitigate and prevent burnout in the medical field.
Vesta Teleradiology is your reliable solution for all your healthcare facility’s radiology requirements, whether you require full-time support or coverage during nights and weekends. With over 16 years of dedicated service to diagnostic imaging centers, physician’s offices, hospitals, and other healthcare facilities, we are here to assist you. Get in touch with us today for a quick quote at 1-877-55-VESTA.
Sources:
Healthcaredive.com
Radiologybusiness.com
Beckershospitalreview.com
Healthimaging.com
Openai.com