Tech in Hospitals Today
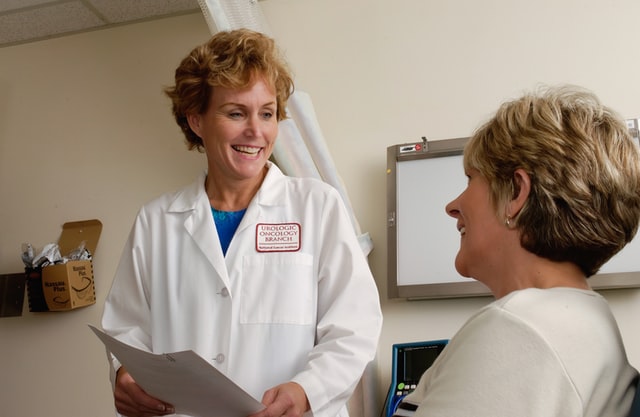
Physicians in private practice continually seek new ways to improve their patient’s care. Technology has provided an efficient and cost-effective way to maximize the delivery of health care services.
Medical communication between primary care, specialists, laboratory analysts, and hospitals has been improved and expedited through the efficiency of mobile technology and online resources.
Staff can update patient charts throughout an entire system with one update. Physicians can prescribe treatment plans within minutes, whereas before, information would sometimes take days.
The medical profession has mostly eliminated paper charts. Unique office organization methods (and some problematic handwriting) are no longer an issue with medical updating.
Technology has also offered physicians the ability to expand their office business using mobile devices and laptops. Physicians can visit and provide updates to their patients who can remain in the comfort of their homes.
Technology has provided physicians the ability to monitor special needs patients at home or in hospital settings without leaving their offices. This ability reduces the possible transmission of disease and infection from sources outside the patient’s environment.
Evolving Technology
Paper replacement and monitoring are not the only promising technology additions that will benefit physicians’ offices in the future.
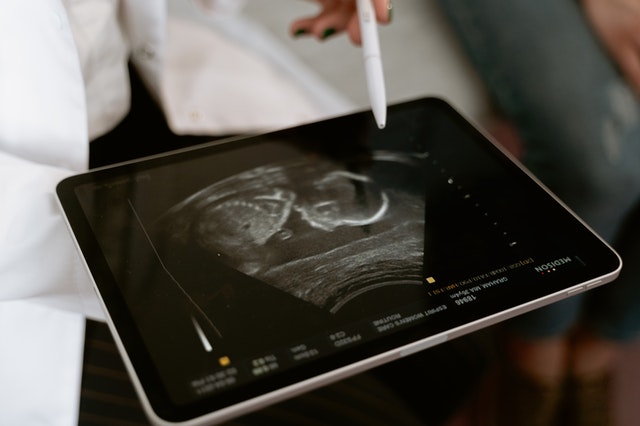
Handheld ultrasound imaging has become affordable equipment. Researchers figured out how to put ultrasound technology into a computer chip rather than a $100,000 machine in a hospital. The program simply connects to an iPhone app.

Faster, more efficient diagnostic information is available within the confines of a physician’s office now. Programs are available that can scan the 2 million peer-reviewed research papers published every year. Clinical trial results and biomedical information can provide a physician with relationships between drugs, disease, and genes within a few minutes.
Digital capture of radiology imaging allows teleradiology reduced records to be transported almost immediately to any specialist with an internet connection. Time-sensitive treatments for head injuries and strokes can be prescribed, and more lives in rural and remote locations will be saved.
The future holds more integration of telemedicine and decision support systems for physicians. Equipment and smaller devices are more affordable to the physicians as well.
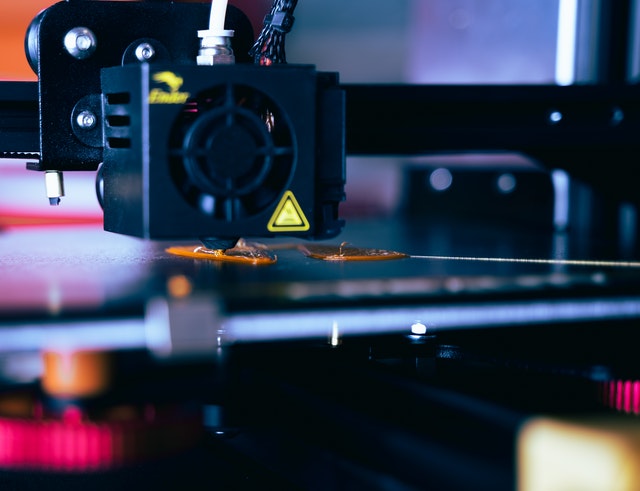
More services such as more complex surgeries may be available to physicians’ offices. With the advancement of telementoring and telerobotic surgeries, physicians may perform surgeries in their offices that would typically be performed in a hospital.

Evidence-based information and technologies can improve patient care, save lives, and save money anywhere and everywhere the internet is available–even from the physician’s office.
Vesta’s Tech Solutions
Vesta Teleradiology wants to improve both your experience as well as your patients’ experience. That’s why we offer tools and customizable reports that work WITH your current workflow as well as offering teleradiology to supplement your current needs. Efficiency, quick turnaround times and US Board Certified Radiologists are what make Vesta a formidable partner for your healthcare facility.











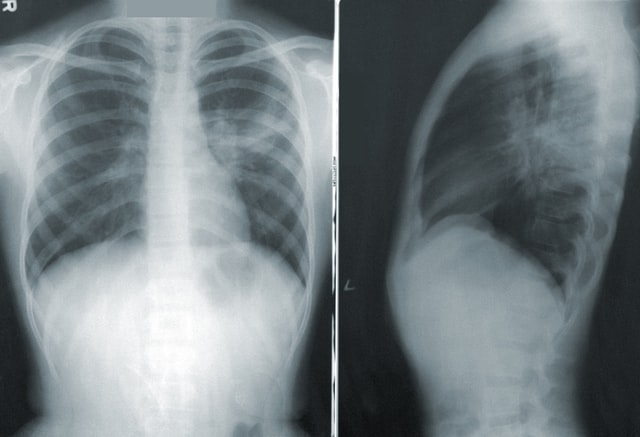


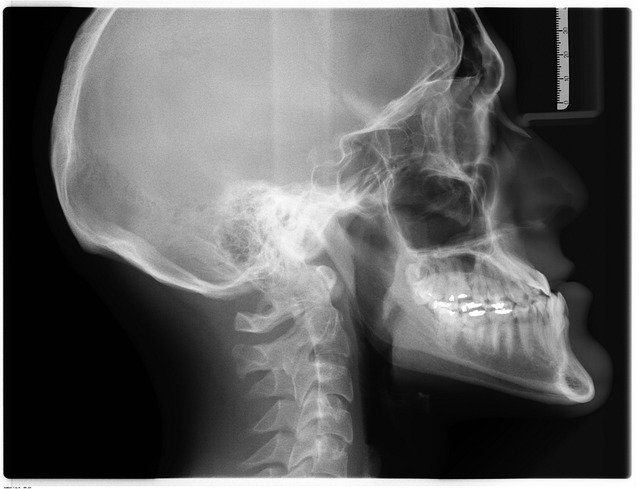 Going back to the beginning, the first X-ray picture in 1895 by
Going back to the beginning, the first X-ray picture in 1895 by
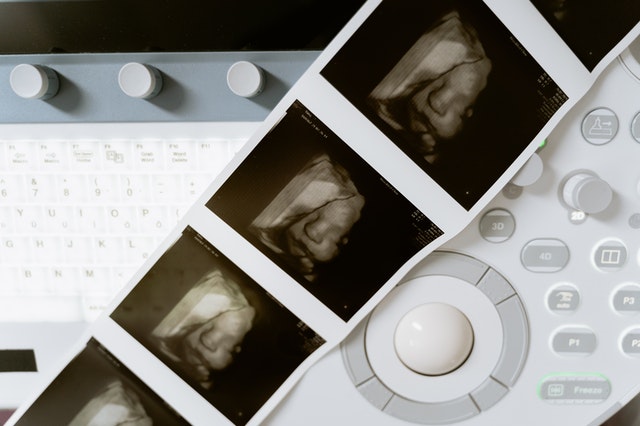 Fun Fact: the 3-D ultrasound actually takes thousands of photos at once to create a 3d image that is extremely clear.
Fun Fact: the 3-D ultrasound actually takes thousands of photos at once to create a 3d image that is extremely clear.



 Studies suggest
Studies suggest