Being told that you need diagnostic imaging can be scary. Healthcare professionals deal with diagnostic imaging every day, so they may become immune to the concerns of patients.
Still, amidst patients’ fear of diagnostic imaging, healthcare professionals can set their minds at ease.
The main thing to remember is to simply treat your patients like humans. Slow down, treat them with kindness, and really listen to their concerns. Doing these simple things can go a long way in setting your patients’ minds at ease.
What Concerns Do Patients Have About Diagnostic Imaging?
One of the most common concerns amongst patients is the claustrophobia caused by MRI machines. Dealing with the tight space of an MRI machine can be very stressful for patients dealing with claustrophobia and anxiety.
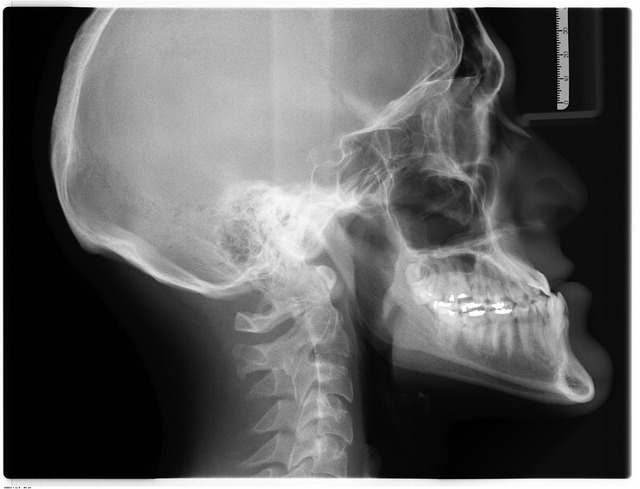
Regarding X-rays, patients are often concerned about their radiation exposure. They fear that the imaging may put them at increased risk for cancer.
Treat Your Patient Like a Person
One of the most common complaints from patients is that they don’t feel like the person working with them is treating them with care and understanding.

Smile and say hello when you first enter the room. Something as small as a smile can instantly put a person’s mind at ease, especially in a clinical setting that is scary for many patients.
Always refer to the patient by their name. Never refer to them as “the patient” while they are in earshot. Doing so sounds cold, while using their name makes the interaction feel more personal.
Maintain eye contact with your patient. Don’t look at their chart so much that you forget to make them feel like they’re being heard. Eye contact can make them less anxious, especially if they’ve been waiting a long time or have specific fears.
Make sure you sit — standing over a seated patient can be intimidating.
Listen & Understand
Health Management emphasizes how important it is to listen to your patient and ask questions. Let them explain what is going on before you begin to speak. Don’t interrupt them. If they have something to add while you’re talking, allow them to interject and listen to what they say.
Giving your patient space to speak can clarify any confusion on both parts.
After they have finished, reiterate what they’ve said to ensure you understand their concerns. Doing so shows the patient that you are interested in helping them and have respect for their situation. It also ensures that both the patient and healthcare provider are on the same page with treatment going forward.
Also, remember to slow down. Many patients feel that healthcare providers are in a rush, that they’re wasting their time, and that the provider would rather be elsewhere. Patients deserve to feel that their time is valued. Slowing down also helps patients to feel like they are heard and understood.
Watch Your Tone
Patients often come to healthcare providers with sensitive information that can make them feel vulnerable. Health Management encourages professionals to speak to patients with a warm, calm tone of voice. It can do a lot to set their mind at ease. Speaking more slowly can do the same.
Educate Your Patients
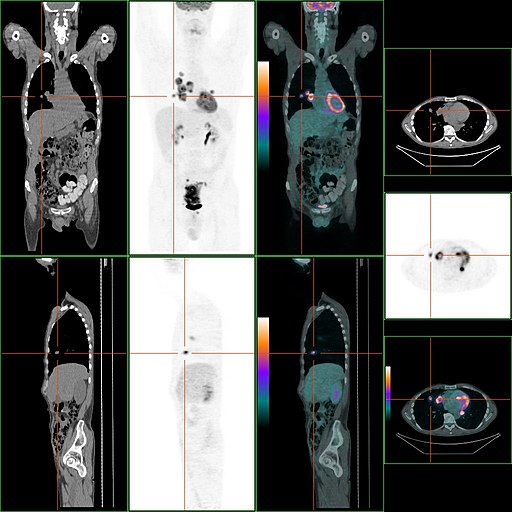
Lawrence T. Dauer et al. say professionals should educate their patients. They should know exactly what’s happening during the imaging and what effects the imaging may have on their bodies.
For example, many patients fear how much radiation they’re getting. Explain that they are receiving very little radiation exposure.
Don’t lie to them. Professionals know that repeated exposure, a person’s age, and other factors may increase risk. Patients deserve to know that, but you can set their minds at ease by explaining their risks.
Patients should always have informed consent. They should know precisely what they’re going into and be okay with it. Consent is not just about getting the patient to sign a form. It ensures they are adequately educated about their procedure and entirely on board.
Be Clear
As a healthcare professional, you know a lot of medical and technical jargon that the patient likely does not. Speak straightforwardly, using familiar words. It is crucial that the patient understands what is going on with their treatment.
At the same time, Health Management warns you to be careful not to come across as patronizing. Although patients may not know medical jargon, it doesn’t mean they’re stupid.
Reducing MRI Claustrophobia Concerns
The University of Virginia says the main reason patients are fearful of MRI machines is because they lack understanding of them. Many professionals can ease patients’ minds by informing them that MRI machines are well-lit and open at both ends. They are not closed off and dark, as many patients fear.

Professionals can teach their patients easy breathing and meditation techniques to help keep them calm during the procedure. Another option is to tell them to count to keep their minds busy or to go to their “happy place.”
Provide them with a towel or washcloth they can drape over their eyes so they can’t see what’s going on.
Provide patients with headphones and allow them to listen to their music of choice.
Talk to your patients — about anything — get their minds off the procedure.
Conclusion
Diagnostic imaging can be scary for patients, especially those dealing with anxiety. Medical professionals are critical in setting a patient’s mind at ease, and it’s not hard to do.
Slow down, treat your patients with kindness and respect, and ensure they are properly informed. These simple things can help calm your patients and help you build a lasting professional relationship.