RSNA’s 2025 theme, Imaging the Individual, isn’t just about futuristic science—it’s about doing the basics better for each patient, every day. The official Trending Topics preview highlights three threads cutting across subspecialties: AI you can deploy, personalized care you can operationalize, and equity you can measure. This guide translates those themes into practical checkpoints hospitals and imaging centers can use right now. RSNA
1) AI that graduates from pilot to practice
This year’s agenda emphasizes real outcomes over proofs of concept: reader-in-the-loop tools, bias monitoring, and governance. In breast imaging alone, RSNA previews spotlight external validation for image-only risk models and integration of MRI signals into multimodal AI—clear signals that “personalization” is landing in routine workflows. Bring vendor questions that force specifics: external validation cohorts, drift detection, and how metrics (TAT, recalls, rework) appear in your dashboard. RSNA
What to set up before RSNA: define 3–5 outcome metrics and insist every demo shows pre/post performance tied to those measures. Use QIBA concepts to push for standardized inputs/outputs so results are reproducible across scanners and sites. QIBA Wiki
2) Personalization that reaches the reading room
Personalization isn’t only radiogenomics. RSNA’s preview points to risk-stratified pathways you can actually run: e.g., image-only 5-year breast cancer risk at the point of screening to route patients into annual vs. short-interval follow-up or supplemental imaging (CEM/MRI). That pairs well with updated U.S. recommendations: screening beginning at age 40 for average-risk women, then adjusting based on risk and local policy. Build routing rules, templates, and letters now, so RSNA demos can plug into your plan.
Operational checklist:
- Map risk thresholds → next steps (annual vs. short-interval, CEM/MRI).
- Standardize templates so risk outputs appear consistently in reports and patient letters.
- Decide who reviews outlier risk flags and how quickly (SLA).
3) Equity you can instrument—not just endorse
RSNA is foregrounding health equity, with sessions on encoding equity in AI and addressing access gaps for underserved communities. Equity becomes real when you can see it in your data: turnaround times by language, missed-appointment patterns by zip code, recall rates by screening site, and AI performance by subgroup. Build those slices into your analytics now; then ask vendors to show subgroup performance in their dashboards.
Practical moves:
- Add demographic and language filters to your TAT and recall reports.
- Require AI vendors to show calibration and error analysis by subgroup.
- Stand up multilingual patient letter templates to support new screening starts at 40. USPSTF
4) CEM/MRI momentum: choose the lever that fits your service line
RSNA coverage calls out CEM as an increasingly practical adjunct—especially useful for dense-breast populations and diagnostic workups where capacity or cost limits MRI. The RACER trial reported higher accuracy and efficiency for CEM as the primary exam for recalled women vs. conventional imaging—evidence that can justify protocol changes and equipment planning. Meanwhile, MRI retains the sensitivity crown, with renewed attention on background parenchymal enhancement (BPE) as a signal worth documenting consistently.
Action items:
- Decide where CEM fits: diagnostic recall pathway, dense-breast supplemental strategy, or both.
- Add BPE level to structured MRI reports and trend it during therapy response clinics.
5) Governance, not guesswork
If personalization is the “what,” governance is the “how.” Use QIBA ideas—claim definitions, acquisition standards, and profile adherence—to control variability across devices and shifts. Tie RSNA learnings to a written governance plan with three parts: 1) protocol book (who owns it, update cadence), 2) quality book (metrics, subgroup views), and 3) AI book (approval process, monitoring, rollback).
6) Where teleradiology extends your capacity
Personalization increases complexity at peaks (recalls, dense-breast seasons, MR backlogs). A teleradiology partner helps you keep individualized pathways moving: standardized templates, subspecialty over-reads, and after-hours coverage that adheres to your risk rules and equity metrics—so “Imaging the Individual” doesn’t stop at 5 p.m.
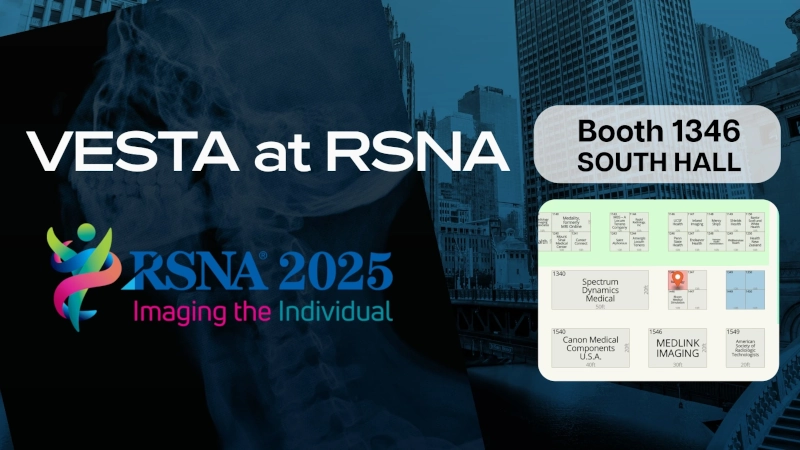
Headed to RSNA?
Visit Vesta at Booth 1346 (South Hall) to see how we make “Imaging the Individual” work in real clinics—then enter to win a 1-year Medality CME subscription. Don’t wait: email “RSNA CME Entry” to info@vestarad.com now for a reserved entry, and show your confirmation at the booth for a bonus entry.


 This challenge is magnified by a growing shortage of radiologists, particularly those specializing in breast imaging. A 2023 workforce survey from the
This challenge is magnified by a growing shortage of radiologists, particularly those specializing in breast imaging. A 2023 workforce survey from the
 This extension is part of CMS’s ongoing efforts to maintain flexibility in healthcare delivery, particularly in response to the challenges posed by the COVID-19 pandemic. Initially introduced in 2020, the virtual supervision policy has been extended multiple times, reflecting its effectiveness in enhancing access to care, especially in rural and underserved areas.
This extension is part of CMS’s ongoing efforts to maintain flexibility in healthcare delivery, particularly in response to the challenges posed by the COVID-19 pandemic. Initially introduced in 2020, the virtual supervision policy has been extended multiple times, reflecting its effectiveness in enhancing access to care, especially in rural and underserved areas.
 Looking Ahead
Looking Ahead
 And for
And for 
 How Vesta Teleradiology Provides Specialized Radiology Support
How Vesta Teleradiology Provides Specialized Radiology Support
 However, challenges remain, including concerns about transparency in AI decision-making and biases in data sets. These hurdles are gradually being addressed with stricter regulations and improved algorithm training. AI isn’t just a tool; it’s becoming a trusted collaborator in radiology practices worldwide.
However, challenges remain, including concerns about transparency in AI decision-making and biases in data sets. These hurdles are gradually being addressed with stricter regulations and improved algorithm training. AI isn’t just a tool; it’s becoming a trusted collaborator in radiology practices worldwide. Radiology practices are adapting to these regulations by enhancing their reporting systems and educating patients about the implications of breast density. This legislation empowers patients to make informed decisions about supplemental screening options, improving early detection and outcomes.
Radiology practices are adapting to these regulations by enhancing their reporting systems and educating patients about the implications of breast density. This legislation empowers patients to make informed decisions about supplemental screening options, improving early detection and outcomes.
